Know Your Germ
Pathogen Compass
It's All About the Pathogen!
Not all substances work equally well for a urinary tract infection, whether natural or conventional antibiotics.
Given the many options and active ingredients (herbal medicines, antibiotics, etc.), it’s worth taking a closer look at the various pathogens involved in urinary tract infections and their targeted treatment.
- How do I treat the urinary tract infection most effectively?
- How do I prevent a relapse (recurrent urinary tract infection)?
- How do I avoid unnecessary antibiotics?
The Sad Truth
When you have a urinary tract infection, you usually encounter the same frustrating process:
The Standard Procedure
-
GP
Typical symptoms | Urine test strips positive
-
Antibiotic
Standard antibiotic
At first glance, the process seems straightforward and often successful if: your urinary tract infection is uncomplicated, the appropriate antibiotic was "guessed" (=> calculated therapy), and the pathogen(s) have not embedded and hidden in your bladder wall.
The sad truth is that the "Standard Procedure" is often ineffective or only briefly successful.
Possible consequences:
- The antibiotic does not work (because it is not effective against the unknown pathogen)
- You receive one antibiotic after another (and your risk of antibiotic resistance increases)
- Your urinary tract infection returns shortly (recurrent urinary tract infection)
The inevitable consequence:
- Unknown pathogen => You do not know the causing pathogens of your urinary tract infection.
Essential: The Antibiogram
If you have failed the "Standard Procedure" and suffer from recurrent urinary tract infections, an important additional treatment step is required:
Urine Culture with Antibiogram
-
GP > Laboratory
Urine sample
-
Antibiogram
Pathogen identification | Antibiotic sensitivity analysis => 2-4 days
-
Sensitive Antibiotic
Effective according to the antibiogram
-
Follow-Up
Urine test strips negative
You might be wondering: Why isn't the gold standard of an antibiogram always used right away?
- Additional time required
- Higher costs
What can you do about it?
- Insist on a urine culture at the time of registration!
- Be persistent!
I Can’t Wait
The urine culture needs to be incubated, which means from the time of urine collection to receiving the antibiogram typically takes 2-4 days.
If your symptoms do not allow for waiting, or if the potential risk of a complicated urinary tract infection requires immediate antibiotic administration, then your treating doctor will have to "guess" and initiate a so-called empirical therapy (as in the simple standard procedure).
In plain terms: You start taking a "best-guess" antibiotic and once the antibiogram (= the "results") arrives, adjustments can be made if necessary, and you switch to a different antibiotic.
Don't Forget: Follow-Up
The important final treatment step is unfortunately often neglected due to convenience: the follow-up.
For the follow-up, it’s best to visit your doctor’s office at the earliest 3 days after the last dose of antibiotics. Alternatively, you can check your urine at home with urine test strips (the doctor usually does the same).
Narrowing Down the Pathogen Without an Antibiogram
There are always reasons why the gold standard of an antibiogram is not used: weekends, travel abroad, being brushed off at the practice, etc.
Not visiting the practice usually means: no antibiotic and self-treatment with home remedies and natural substances (Note: Know the limits).
What Matters
Particularly when using naturally antimicrobial substances, it’s worthwhile to narrow down the pathogen to a specific characteristic: gram-positive or gram-negative.
Whether gram-positive (thick peptidoglycan layer) or gram-negative (thin peptidoglycan layer) makes a significant difference in treatment with natural remedies.
- The growth of gram-positive pathogens should be inhibited by acidic urine.
- The growth of gram-negative pathogens should be inhibited by alkaline (=basic) urine.
Self-Test "Baking Soda"
This is how you can try to determine whether you have a gram-positive or gram-negative infection.
-
Dissolve 1/4 teaspoon of baking soda in water and drinkDo not eat for 2 hours before
-
Wait 40 minutesThis is approximately how long it takes for the baking soda water to reach your bladder
-
Symptoms worsen ==> gram-positive Symptoms improve ==> gram-negativeSymptoms unchanged ==> possibly not a UTI (but e.g. a vaginal infection)
Self-Test "Nitrite"
With the help of a urine test strip, you can find out if your pathogen produces nitrite in the urine. Nitrite-producing pathogens are almost always gram-negative.
-
Urine test stripDo not empty your bladder for 4 hours beforeAvoid contamination: wash beforehand, mid-stream urine
-
Adhere to reading time (usually 1-2 minutes)Follow the package instructions exactly
-
Nitrite test field negative ==> gram-positive Nitrite test field positive ==> gram-negative
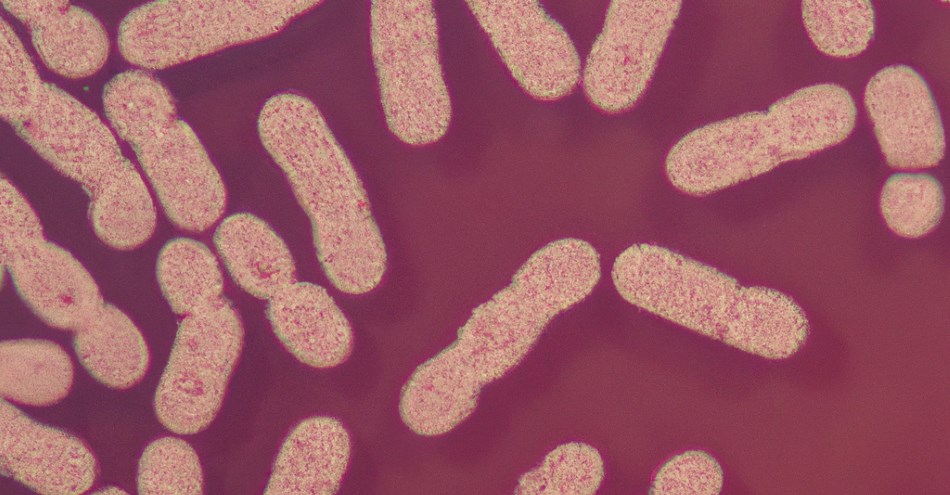
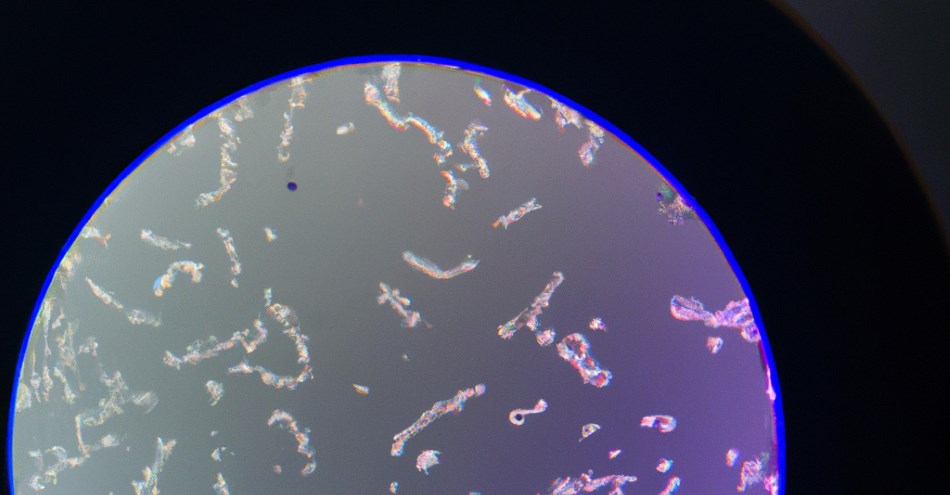
Gram-Negative Pathogens
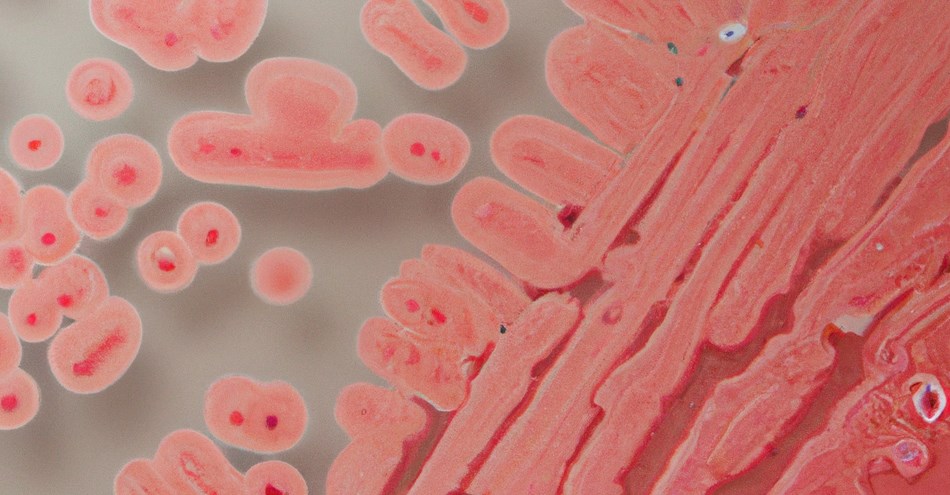
Pathogen spectrum of gram-negative pathogens of acute cystitis in women in Germany.
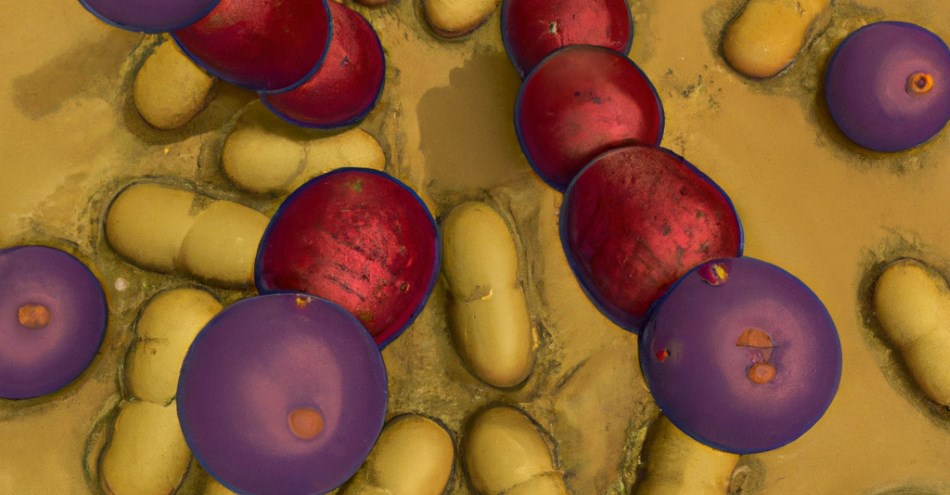
Gram-Positive Pathogens
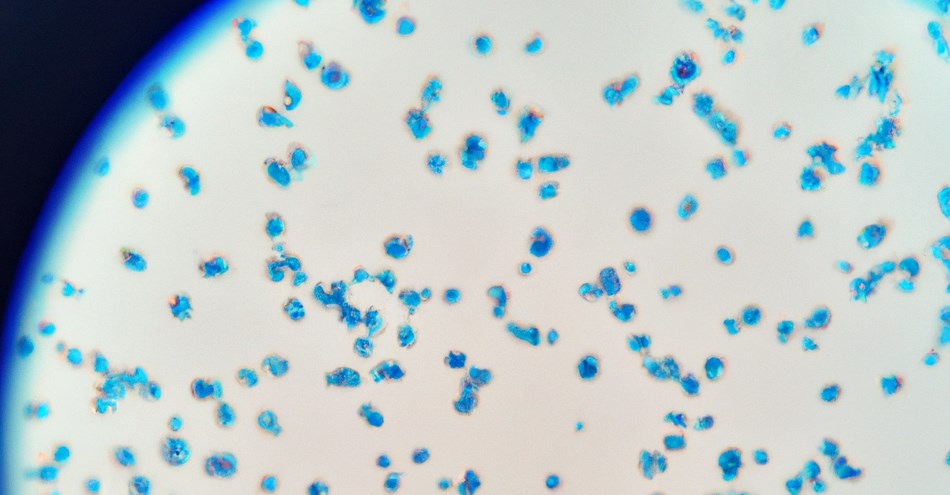
Pathogen spectrum of gram-positive pathogens of acute cystitis in women in Germany.
Mixed Infection from Gram-positive AND Gram-negative
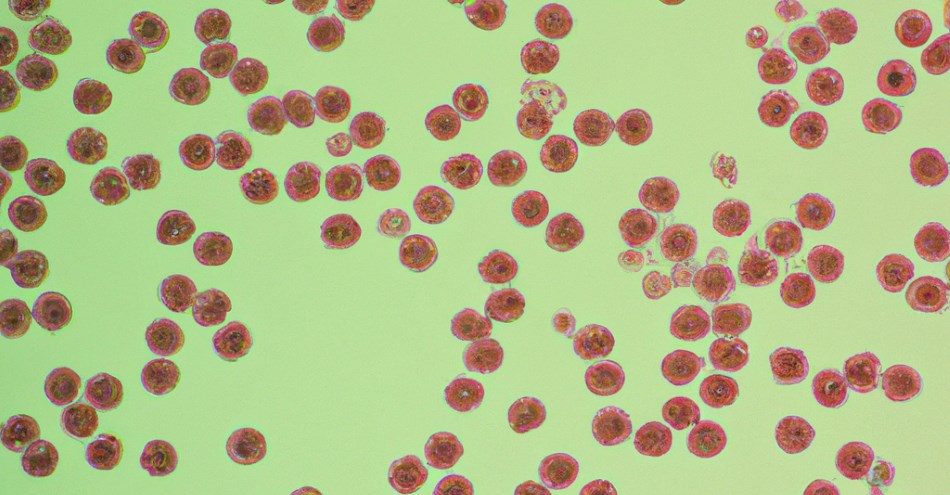
A mixed infection is not uncommon and very often it is a combination of gram-negative and gram-positive bacteria.
In this case, it is recommended to treat the potentially "more dangerous" germ first.
Gram-negative bacteria pose a higher risk, as they can almost invariably "swim" with their flagella and thus ascend to the upper urinary tract (e.g. kidneys) much faster.
The bacterial count also plays a role in the assessment. When the bacterial count reaches 10^5, it is referred to as a "fully developed" bladder infection.
In addition, the threat posed by gram-negative, multi-resistant bacteria has steadily increased in recent years, such as the ESBL-producing E. coli. It is no longer just the multi-resistant MRSA (Methicillin-resistant Staphylococcus aureus) that causes difficult-to-treat infections.
Atypical Pathogens: Mycoplasma, Chlamydia & Co.
You suffer from the typical symptoms, but even the urine culture doesn't find any bacteria? Then it could be that you've contracted a sexually transmitted pathogen. These pathogens require a special culture and cannot be detected with the standard urine culture procedure.
Natural Antibiotics
There are many natural home and herbal remedies for bladder infections – probably even too many. So how do you best navigate the jungle of remedies for bladder infections?
Of course, you are welcome to try everything (if your wallet can handle it in the long run), BUT:
Not every active substance can equally attack all urinary tract pathogens.
However, to avoid missing the bigger picture, I would like to introduce you to what I believe are the most important natural antibiotics along with their spectrum of effectiveness. This, of course, doesn't mean that other remedies are ineffective – and what works for you personally is always right.
Now that you know your pathogen from the antibiogram or have clues about your pathogen group (gram-positive / gram-negative) from self-tests, you can also target your treatment much more effectively with a combination of natural remedies.
Start here! Use the filter bar to search by pathogen group or remedy. A click on the round filter icon in the bottom left will quickly take you back to the filter bar.
Note: The images of the individual pathogens are exemplary and make no claim to accuracy.
Biofilm Breakers
The term biofilm refers to bacterial colonies that protect themselves from attacks by the immune system and other substances such as antibiotics through a self-produced extracellular polymeric matrix.
Embedded pathogens, which hide in the bladder mucosa and also live in a biofilm-like community, behave very similarly.
To combat bacterial hiding places, there are various approaches:
- Forskolin to dissolve the intracellular embedding of germs. Alternatively: Chitosan acts as a bladder wall exfoliant (removes the superficial layer of bladder cells).
-
Biofilm Inhibitors:
- Phytopharmaceuticals: e.g. Cress and Horseradish (Angocin® Anti-Infekt N*), Arbutin (from bearberry leaves), Coumarins. Angocin® Anti-Infekt N* (Cress herb and horseradish root) works antimicrobial due to the included mustard oils. Numerous studies support the pronounced germicidal effect of isothiocyanates (ITC, mustard oils). Bacterial growth of multidrug-resistant germs and even the formation of resistant biofilms can be inhibited.
- N-Acetyl L-Cysteine (NAC): antioxidant, anti-inflammatory, and mucolytic (mucus-dissolving), destroys and reduces the formation of biofilms by bacteria and fungi.
- Lactoferrin: The enzyme Lactoferrin deprives bacteria of the vital nutrient iron, thus preventing biofilm formation (bacteria constantly seek nutrients). Lactoferrin is an endogenous peptide found in tears, saliva, and breast milk.
- Enzymes (e.g. Nattokinase, Serrapeptase): Interfase® Plus - Klaire Labs, Biofilm Defense® - Kirkman®
- Long-Term Antibiotic Therapy in combination with the urinary tract disinfectant Hiprex®
- Phage Therapy: Phages are viruses that attack and dissolve bacteria (also in biofilms and also dormant bacteria known as persisters). Phage therapy is still practiced in the countries of the former Eastern Bloc. Phages are host-specific, meaning they act specifically on a bacterial species.
Sources
https://pantrypharmacy.com/category/the-kill-list-series/
https://register.awmf.org/assets/guidelines/043-044l_S3_Harnwegsinfektionen_2017-05.pdf
https://www.deutschesapothekenportal.de/download/public/fortbildungen/dap_fortbildung_blasenentzuendungen.pdf
https://www.iqwig.de/download/ht20-01_pflanzliche-mittel-bei-blasenentzuendung_hta-bericht_v1-0.pdf
https://www.egms.de/static/de/meetings/urobay2018/18urobay062.shtml
https://edoc.ub.uni-muenchen.de/26613/1/Magistro_Giuseppe.pdf
https://www.uni-ulm.de/fileadmin/website_uni_ulm/iui.gesfuermit/Newsletter/Newsletter_Sommer_2017.pdf
https://www.pharmazeutische-zeitung.de/ausgabe-032015/gemeinsam-zur-attacke/
https://bellalindemann.com/blog/treat-uti-naturally-without-anitbiotics
https://www.deutschlandfunk.de/geknackte-gemeinschaft-100.html
https://www.pagepressjournals.org/index.php/aiua/article/view/aiua.2017.1.45/6474 (Prospective study to compare antibiosis versus the association of N-acetylcysteine, D-mannose and Morinda citrifolia fruit extract in preventing urinary tractinfections in patients submitted to urodynamic investigation)
https://www.stoputiforever.com/treatment/bacterial-biofilm-treatment-uti/
https://www.sciencedirect.com/science/article/pii/S095461111630141X
https://encyclopedia.pub/entry/12723
https://www.pharmazeutische-zeitung.de/ausgabe-072009/cumarine-in-pflanzlichen-arzneimitteln/
https://www.management-krankenhaus.de/news/aktuelle-studie-der-universitaet-heidelberg-zu-biofilmen
https://www.deutsche-apotheker-zeitung.de/news/artikel/2018/01/01/cystinol-baerentraube-bei-blasenentzuendungen
https://www.apotheken-umschau.de/krankheiten-symptome/nieren-und-harnwegserkrankungen/das-hilft-wirklich-bei-einer-blasenentzuendung-717367.html
https://www.pharmazeutische-zeitung.de/ausgabe-352007/brennpunkt-blase/
https://www.uniklinik-freiburg.de/presse/publikationen/im-fokus/urologie-hilfe-fuer-die-entzuendete-und-gereizte-blase.html
https://www.blasendoktor.de/
https://urosurf.elearning.aum.iml.unibe.ch/theory/nitrite1.html?urosurf%7Ctheory%7Cchemanal%7Cnitrite%7C1
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8066587/
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001321.pub5/full
https://www.researchgate.net/publication/323167475_ANTIBACTERIAL_ANTIFUNGAL_POTENTIALITY_OF_RICINUS_COMMUNIS_COLEUS_FORSKOHLII_ON_SOME_HUMAN_PATHOGENIC_MICROORGANISMS
https://www.pharmazeutische-zeitung.de/alternativen-zu-antibiotika-134532/
http://publications.rwth-aachen.de/record/781590/files/781590.pdf
https://www.pharmazeutische-zeitung.de/antiseptikum-als-alternative-zu-antibiotika-131844/seite/alle/
https://www.angocin.de/angocin/wirkung-senfoele
https://www.springermedizin.de/harnwegsinfektionen/zystitis/unkomplizierte-harnwegsinfektionen/18278812
https://www.deutsche-apotheker-zeitung.de/daz-az/2012/daz-44-2012/kapuzinerkresse-ist-arzneipflanze-des-jahres-2013
Cystitis Unmasked, Malone-Lee, J
Alles was Du wissen musst um Deine wiederkehrende Blasenentzündung für immer los zu werden, Theresia Niedermeier
Blase gut ... alles gut! Prof. Dr. med. Stephan Roth