FAQ UTI
Answers to all questions about urinary tract infections
Hydration
Sounds daft, but "wait and drink tea" is quite apt. Best to have unsweetened tea (bladder and kidney teas made from nettle, birch leaves, goldenseal, quack grass, uva ursi, juniper berries, and dandelion root) or still water. Herbal diuretics cleanse the urinary tract and help eliminate pathogenic bacteria without affecting electrolyte balance.
If you can't get the tea from a pharmacy, then there are pre-mixed products (tea or granules) available, e.g. Harntee 400 TAD N*. Warning: According to Ökotest, bladder teas are consistently failing due to alarming contamination with pyrrolizidine alkaloids (PA) and pesticides. Better options are bio-quality teas made from single types of herbs, e.g. Horsetail Herb*.
My go-to for cleaning out the system: Heumann Bladder and Kidney Tea Solubitrat Uro* for dissolving - nice and easy.
My choice for prevention or when I'm too tired to have tea: tap water (with D-Mannose*. if the triggering bacteria is E. coli).
If you simply can't abide by tea, then there are herbal supplements available in capsule form, more on this in Drink & Flush.
Opinions on this are very different, even among experts. However, it's not a blanket statement that more fluid always brings more.
One view is: "Antibacterial substances in urine become diluted when drinking too much." On the other hand: "Drainage can indeed be a way to get rid of bacteria, as the immune system has already failed with an infection." Immunisation
Warning: During treatment with antibiotics, you should avoid excessive drinking, as this reduces the concentration of antibiotic in the bladder and makes it less effective.
Prevention is sensible: A study by the University of Miami has proven the effectiveness of increased fluid intake to reduce the risk of recurring urinary tract infections. The women in the test group drank an additional 1.5 litres of water for 12 months, on top of their usual fluid intake (less than 1.5 litres).
My personal experience: I find drinking a lot usually helps me. However, I mean up to 3 litres per day. Some people overdo it and then get into trouble.
As a general rule, it's recommended to drink 1.5 to 2 litres of fluid per day. You may need more if you have a high energy expenditure, are in a hot environment, or are experiencing symptoms such as fever, vomiting, or diarrhoea.
When taking antibiotics for an acute urinary tract infection, it's essential not to drink excessive amounts of fluid, as this can dilute the concentration of the medication in the bladder.
Be aware that drinking too much fluid can lead to false-negative results when using urine sticks. This is because the concentration of white blood cells may be lower and/or the by-products of bacterial breakdown (nitrite) may not yet be detectable.
Yes, it can. You might be trapped in a vicious cycle of infection and irritation. The contraction of the inflamed bladder lining when you go to the loo irritates the lining even more => that's why peeing becomes so painful at the end.
I also often read that many sufferers take a mix of various herbal remedies at the same time. This is usually well-intentioned, and there are countless products available on the market, but taking a multitude of herbal medicines and excessive drinking can certainly cause damage and irritate the bladder.
Drinking enough water is very important, but many sufferers overdo it with the quantities. Drinking litres upon litres might be well-intentioned, but usually doesn't bring the success they hope for.
Typically, alcohol and coffee irritate the urinary tract through their acidity and can exacerbate symptoms of a urinary tract infection.
Alcohol promotes inflammation, widens blood vessels, and particularly irritates the mucous membrane. This alone can be enough reason for your bladder to become sensitive.
My tip: You don't have to give up everything if you're careful to drink enough water at all times. For example, my bladder reacts sensitively to pure red wine, but I have no problems with a white wine spritzer. Coffee doesn't bother me either, as long as I dilute it with enough water afterwards.
Coffee, alcohol and orange juice in particular can irritate the bladder further due to their acidity. Try fizzy drinks to see if they agree with you.
My experience: Diluting drinks with enough water tends to result in fewer bladder complaints. Fizzy drinks don't tend to suit my bladder (especially when it's inflamed).
There are conflicting opinions on this matter. According to the medical S3 guidelines, the study findings are contradictory, and therefore no recommendation is made for consuming cranberry products (capsules, tablets, juice or syrup). The effectiveness of these products has not been proven - which is generally quite difficult with herbal remedies.
As a preventive measure to avoid recurring infections, one could try high-dose cranberry. The assumption is that the tannins present in cranberries protect the urinary tract and bladder walls from bacterial infection by preventing bacteria from adhering to the mucous membrane of the urinary tract.
If you give credit to an American website (The Pantry Pharmacy devotes extensive coverage to this topic), cranberry may even exacerbate an infection with E. coli (or other gram-negative pathogens).
From my experience: During an acute urinary tract infection, cranberry products were probably too weak to show any effect in my case. For me, they were simply not a success story. I'm not trying to dissuade you from trying cranberry as a preventative measure - it may be beneficial for your overall health. It's unlikely to cause harm, but may only affect your wallet.
The Federal Institute for Drugs has recognised alkaline mineral water as an effective supportive treatment for urinary tract infections.
The official recommendations are: "For E. coli infections, a sulphate-rich mineral water (with at least 1,200 mg of sulphate per litre) is recommended to acidify, and for other infections, a hydrogencarbonate-rich mineral water to alkalise. For unclear infections, a carbonated mineral water is recommended."
My opinion: One can always do what they want - alkaline water is certainly a healthy alternative to tap water. If you're willing to spend money on health, then go for it. Otherwise, I would invest my money in more promising treatments (such as Forskolin*, D-Mannose*, and/or Angocin® Anti-Infekt N*). Moreover, people disagree about whether acidifying with sulphate-rich water is beneficial or even counterproductive for E. coli infections.
That the topic of cow's milk has taken up whole shelves, you probably haven't missed that. In TCM it is definitely not on the menu.
A study at Oulu University in Finland involving around 300 women found that the risk of urinary tract infections can be reduced by an average of 80% if milk products (yogurt, cheese) are consumed at least three times a week. It is suspected here that the probiotic bacteria beneficial to the gut health and therefore the immune system. Immune System
Warning! Ready-made products, such as fruit yogurts, avoid them: the emulsifiers E433 and E466 often added to food to improve consistency and shelf life are suspected of promoting inflammation in the body's mucous membranes.
So: If you're a fan of cow's milk, just stick with it. If you think cow's milk is bad for you, then leave it out altogether.
This substance, which makes the urine alkaline (pH above 8), is unfortunately not only useful but can also have a negative effect.
On the positive side: I haven't tested it myself yet, but dissolving one quarter of a teaspoon of baking soda in water and drinking it may help alleviate the burning sensation. This solution neutralises the acid in the bladder and relieves the painful symptoms associated with acute cystitis. Another indication of alkaline urine is given when taking arbutin from bearberry leaves. In order for this plant-based disinfectant to form hydroquinone, which has antibacterial properties, the urine must be slightly alkaline.
But be careful: Alkaline urine can attack the epithelium of the urinary tract and promote the growth of certain bacteria (some bacteria survive better in alkaline urine). Additionally, there are pathogens (from the genus Proteus) that increase the pH value of the urine. If you really want to know how it is with your urine's pH level, simply check with indicator paper (such as Uralyt or Neutralit).
If you orientate yourself towards an American website (The Pantry Pharmacy devotes a lot of attention to the topic of urinary tract infections), then alkaline urine is helpful in cases of infection with E. coli (or other gram-negative pathogens). However, if infected with gram-positive pathogens (e.g. enterococci, staphylococci), the urine should be acidic and baking soda should not be taken.
Conclusion: Don't use baking soda too often as a trick against the symptoms. In doubt, keep an eye on the pH value with test strips. An overdose of sodium bicarbonate can even lead to serious poisoning.
Bladder Emptying
As a general guideline, the bladder should be emptied completely every 2-4 hours. Rule of thumb: aim to pass at least 1.5 litres of urine per day. It's essential to remember: when you feel the urge to urinate, go to the toilet and don't delay your visit.
During an acute bladder infection, opinions among experts unfortunately vary greatly. Some recommend emptying the bladder whenever you feel the need, even if it's painful each time. Others advise against frequent urination – urine contains anti-inflammatory substances that should not be diluted too much.
If you're treating your bladder infection with an antibiotic, make sure to only empty your bladder as needed. Frequent urination could cause the antibacterial agents to be eliminated too quickly.
Do you have an overactive (weak) bladder? In that case, bladder training might be something for you. This involves trying to train your bladder according to a specific schedule.
Some doctors say: go to the toilet every time you feel the need to urinate (even if it hurts). Others claim: urine contains antibacterial agents and should not be diluted by excessive drinking or emptied too frequently.
My personal experience: the truth lies somewhere in between. Don't overdo it and go to the toilet a few minutes apart, dripping is irritating the inflamed mucous membranes even more. If I go too infrequently, it burns from the concentrated urine.
Be careful when taking medication too: the active substances in antibiotics or other preparations (such as antibiotics or D-Mannose*) should stay in the bladder to take effect before being eliminated.
This can be checked by a urologist/urogynae with a residual urine ultrasound. During this ultrasound examination, the bladder is measured and the amount of urine remaining in it after urinating is determined.
You yourself can also test this. After emptying your bladder, get up or gently lift your belly button with your fingertips. Then try to empty your bladder again. If more urine comes out then, that's a sign of residual urine in the bladder. Frequent urination can also be a sign of residual urine, as the bladder is refilled faster due to the presence of residual urine.
What's the problem with residual urine? The remaining urine in the bladder allows bacteria and germs to settle and multiply more easily. The risk of infections such as cystitis increases.
It can become problematic when the amount is around 100ml in adults.
A healthy bladder empties completely with each toilet visit. This is ensured by the detrusor muscle contracting, while the two ring-shaped sphincter muscles open. Residual urine then remains in your bladder if the emptying process is impeded.
To fully empty the bladder, you need to relax your pelvic floor and allow urine to flow freely. You can also try:
- Waiting for a moment after urinating, then trying again may increase the chances of emptying the bladder.
- It may also help to stretch the urethra, so that no urine is left behind.
- Getting up and sitting down again, then trying again may be helpful.
- As I suffer from a bladder prolapse (cystocele), I find it helpful to gently push my bladder upwards with my fingertips after urinating, before trying again.
Experimenting may help you find the best strategy for emptying your bladder completely. Note: Do not try to 'squeez' out the last drops.
When you have a urinary tract infection, the lining of your bladder (the urothelium) becomes irritated or inflamed. This makes your bladder less stretchy and it signals the urge to pee much sooner.
Not always is a bacterial infection the reason for constant urges to urinate. Conditions where the bladder is irritated without a clear cause are also known as an "overactive bladder". This can manifest itself in frequent and uncontrollable urges to urinate, often with small volumes of urine. A cause for an overactive bladder is irritation of the vegetative nervous system responsible for bladder control.
The exact causes of an overactive bladder are often unclear. However, conditions such as acute infections and obstructions (kidney stones, tumours) in the urinary tract region must be ruled out. Also, problems with the lumbar spine can lead to an overactive bladder.
In cases of obstructive emptying disorders, removal of the underlying blockage by surgical intervention is often possible. In cases of neurogenic bladder emptying disorder, a medication therapy (e.g. Botoxin injections) may be attempted.
To reduce the symptoms of an overactive bladder or irritation, general measures such as stress relief, giving up smoking, coffee and alcohol can help. Additionally, pelvic floor training is recommended (more information on pelvic floor exercises). These relaxation and tension exercises have a positive effect on the bladder in many cases. Delayed urination by a few minutes can be achieved through so-called bladder training. When the bladder signals its need to be emptied, the toilet visit is postponed for a short time.
As a next step, "bladder dampening medications" (anticholinergics) may be tried.
If medication also does not bring relief, botulinum toxin therapy can provide relief. In an endoscopic procedure, the nerve poison is injected under the bladder wall. The dampening effect lasts for six to nine months and the treatment needs to be repeated afterwards.
When you leak urine when coughing, sneezing, lifting weights or exercising, a doctor refers to it as stress incontinence. This occurs independently of the need to urinate and is usually caused by weakness in the pelvic floor muscles and bladder sphincter.
The causes are often related to age, obesity or pregnancy/birth - although they may have ceased.
Possible treatments include: Pelvic floor exercises, weight loss if overweight, medication and in some cases surgery.
A tip from my gynaecologist that also works well: When you cough or sneeze, turn your head to the side - it automatically tightens the pelvic floor.
Normally, there is no direct transmission of cystitis via the toilet. More often than not, it's an indirect transmission through poor hand hygiene. The bacteria can spread from contaminated surfaces (door handles, loo rolls, soap dispensers, taps) onto your hands. Then, you can transfer the bacteria to the genital area – inserting tampons, your partner's fingers, etc.
Close the cistern before flushing! This is a precautionary measure. Every flush whips up tiny water droplets (aerosols) from the toilet water, spreading bacteria and viruses around the surrounding areas (e.g. loo roll, towel). My tip: On public toilets simply wipe with a tissue from your own handbag.
The best protection is to practice good hand hygiene. This also applies to your partner before you become intimate together.
Wash your hands before and after, avoid scented toilet paper, don't use toilet paper from public toilet, clean yourself from front to back. Use baby wipes only for the anal region!
Heat
Warmth. Although you may sometimes hear the misconception that bacteria thrive on a warm environment and therefore, the bladder should not be treated with warmth during cystitis. Keeping the body warm also promotes good circulation, which in turn supports a good immune response. Additionally, heat has a relaxing effect and helps to reduce pain.
The old-fashioned hot water bottle or a hot-water bottle cushion can therefore still be useful in treating cystitis.
Warmth ensures good circulation to the bladder lining. A well-circulated lining is generally better equipped to deal with infections. Preventative warmth: a poorly circulated skin is often unable to prevent an initial cystitis infection.
Warmth for an acute case of cystitis: warmth boosts the immune system in its fight against bacteria. It also helps relax the lower abdominal area around the bladder, alleviating the often cramp-like pains.
Cold can indirectly trigger a bladder infection. When our body is exposed to cold, the blood vessels constrict and blood flow worsens. If there's already an increased bacterial load and poor blood circulation, the infection can easily rise up into the bladder. In other words: The actual cause lies not in cold feet but rather in pathogens that are more likely to enter the body under these conditions.
My experience: When you're fighting recurring bladder infections, cold often makes it easier for bacteria to take hold. And voilà, the bladder is once again inflamed.
I know it sounds a bit far-fetched at first, but there is actually a scientific explanation for why cold feet might be linked to cystitis. When we're exposed to cold temperatures, our body prioritises keeping the core warm, so that vital organs remain safe. As a result, blood flow in the pelvic area slows down, which can cause localised weakness in the immune system (the mucous membranes are responsible for protecting us from infection). Localised weakness means that bacteria can more easily travel into the urinary tract.
Cold temperatures on their own don't actually cause cystitis; it's the bacteria that take advantage of the weakened state of the mucous membrane that's the issue.
Long story short: If bacteria are already present, standing or sitting on cold surfaces can make cystitis more likely. Wearing damp or chilled clothing, especially around the nether regions, is also not ideal if you're prone to cystitis.
Cold temperatures slow down blood circulation in the pelvic area, which can reduce immunity in this body region. Therefore, it's essential to keep feet and the pelvic area well wrapped up. You should also avoid sitting on a cold surface.
Wearing warm socks or slippers at home. Keeping your lower half covered while sitting in front of the computer or TV.
Keeping the pelvic region warm, for example with kidney warmers tubes*.
Using a heated seat cushion, such as the Thermo Sitzkissen*.
Changing into dry clothes as soon as possible, even if it's a hot summer day.
Always have a warm jacket or coat with you (in the boot, backpack, or tied around your waist)
Wear functional clothing and pack dry spare underwear in your rucksack when engaging in sport and walking activities.
When sitting in cold environments (e.g. at work) use a heated seat cushion. If no power outlet is available, there are also heated cushions with USB connections that can be powered by a standard power bank, such as: USB heated cushions*.
For standing activities in cold environments, you can help yourself with thermopads. Thermopad toe warmers* are so small and handy that they can even be worn in your underwear and placed exactly over the pubic bone. 8 hours of pleasant warmth are thus guaranteed.
Moist heat penetrates a little deeper into the body. That's why moist-heat packs/wraps are ideal. Soak a cotton cloth (about 15x15 cm) in strong chamomile tea (which has a relaxing effect), wring it out and apply to the cyst region. Place a hot water bottle on top and leave for 20 minutes. Then rest.
Alternatively, you can work with sit baths. More information can be found in my article on heat.
Not everyone is a fan of moist heat when it's uncomfortable down there. I'm one of them. I prefer to use hot water bottles ormarshmallow pillows*
Soaking cloths made from cotton fabric, the size of a fist (approx. 15x15 cm). Brew a strong tea / decoction with Sarsaparilla root (which has a relaxing effect), soak the cloth in it and apply to the affected area for 20 minutes. Using a hot water bottle over the cloth allows for even heat distribution. Give the body time to recover afterwards.
Yes, this is possible. There are various reasons why this might happen: increased entry of bacteria through warm water, chilling the lower body, germs outside of the bathwater, etc.
More information can be found at Can I go swimming with a bladder infection?
The warm water at the spa relaxes the muscles in the urinary tract. This muscle relaxation leads to a greater influx of bathwater - and possibly also bacteria.
Whirlpools or saunas often have a high bacterial load and increase the risk of developing a urinary tract infection. As an example, I know someone from a support group who has been fighting a persistent and recurring infection for years after visiting a Hungarian spa.
More on this can be found at Can I go swimming if I have cystitis?
Swimming or bathing is not recommended during a bout of cystitis.
What's more, in coastal areas the water quality may be affected by agricultural runoff and sewage, which can increase the risk of urinary tract infections.
When it comes to lakes and rivers, the water quality is also something to consider. You can usually find up-to-date results of bathing water tests online. In general, river beaches are more susceptible to weather-related changes. After heavy rainfall, for example, there may be a significant increase in bacteria entering the water from the land or sewage treatment plants.
River water is traditionally considered more problematic when it comes to quality, as pollutants can accumulate along longer stretches of water. Heavy rain showers could bring stronger, time-limited bacterial pollution.
More information can be found under Can I go swimming if I have cystitis?
If you're prone to cystitis, it's generally best to have a shower. Soaking in a warm bath can cause the muscles in the urinary tract to relax, allowing bacteria (usually from your gut) to flow into the bladder. If you do take a full bath, make sure to empty your bladder completely afterwards. This will help flush out any bacteria that may have entered the bladder.
Regularly change your bath towel or hand towel and wash it at 60°C. I also like to dry my intimate area with a cotton cloth (or flannel) after each drying, then put it in the washing machine.
Relaxation
It is sensible and important to give your body a break, allowing the urine infection to heal. Rest supports our own bodily defences and can prevent a complicated kidney condition from developing.
When lying down, the bladder receives optimal blood flow and relaxation. Additional warmth also helps with healing.
When lying down, the bladder is optimally perfused and relaxed. Additional, even heat also supports healing. So your immune system works most efficiently, and your body can overcome and heal the infection more effectively.
Back to bed or the sofa. Dry heat with a hot water bottle/moist heat pack etc., or warm baths (increasing temperature) or wraps.
When you have a bladder infection (cystitis), it's advisable to take a break. Exerting yourself too much can be stressful for your body and temporarily weaken your immune system. Therefore, if you have an acute bladder infection, you should not further burden your body with exercise – it needs all its energy to fight off the infection.
As a preventive measure, moderate exercise or simply being physically active in everyday life is ideal. Trained individuals generally have more anti-inflammatory immune cells. Even 20 minutes of moderate activity (a brisk walk, etc.) can slow down inflammatory processes.
That's my tip: At times when bladder infections recur, exercise is beneficial. It doesn't have to be 'exercise' as such – rather incorporate more physical activity into your daily routine.
D-Mannose
The sugar molecules of the simple sugar extracted from maize or birchwood block the finger-like anchors of bacteria that have entered your bladder and make it harder for them to adhere to the urothelium (= multi-layered lining of the urinary tract). The pathogens can no longer attach themselves to your bladder wall, but are simply flushed out with the next urination.
Since D-Mannose* is hardly metabolised, you can also take D-Mannose as a diabetic. D-Mannose* has no effect on blood sugar levels - a large part is excreted in the urine without being digested.
When manufacturing D-Mannose* (sum formula C6H12O6), glucose is extracted from maize or birch via multiple production steps to produce D-Mannose*. Whether birch or maize is used as a source, the end product has the same chemical formula.
Maize has the advantage of being a fast-growing crop compared to birch wood. However, it also often comes with the disadvantage of being sourced from genetically modified crops.
D-Mannose* made from birch is generally more expensive, but many of my fellow sufferers claim it has a better effect (although this cannot be proven chemically).
This question can't be answered so easily, but you can keep an eye out for a few criteria when searching through the many different supplements:
- Pure D-mannose* (100%) is best in powder form
- No additives such as sugar, cranberry or vitamins
- When from maize, please ensure it's from non-GMO cultivation
- Check the quality: Is a lab certificate available from an external lab? Made in Germany?
- Expensive is not necessarily better!
Don't be swayed by expensive combination supplements (I won't mention any brands here ...). Powder form is the cheapest and best, but I also have them in tablet form for when I'm on-the-go. Always stocked up with: Natural D Mannose Powder ZeinPharma* or D-Mannose*
Almost everywhere online, people are saying: D-Mannose helps with infections. But at which ones does it actually help?
Firstly, D-Mannose is not effective against Proteus Mirabilis, E. coli, Klebsiellen, Enterokokken, Staphylokokken, Pesudomonas or Gonokokken.
To check if your infection can be treated with D-Mannose, you can perform a urine test using a nitrite strip (see below for more information).
If the strip shows nitrites, it is likely that the bacteria are E. coli, Klebsiellen or Proteus Mirabilis, and D-Mannose may be effective.
However, if the strip does not show nitrites, it could indicate that the bacteria are not sensitive to D-Mannose (Enterokokken, Staphylokokken, Pesudomonas or Gonokokken).
In such cases, using D-Mannose would not be effective.
It's worth noting that the nitrite strip may sometimes produce false results. You can try using D-Mannose at the beginning of your infection to see if it helps. If it does, great! If not, then it is likely that D-Mannose is not effective against your specific type of bacteria.
D-Mannose* is a sort of wonder cure, which is very effective and, at the same time, has no (known) side effects. The simple sugar is produced in small quantities by the human body itself, so it's essentially a natural substance.
In cases of individual intolerance or extremely high doses, D-Mannose can cause gastrointestinal discomfort. It's also worth noting that D-Mannose may not be suitable for people with certain medical conditions, such as diabetes or kidney disease.
Interactions: D-Mannose* does not interact with the effects of food supplements or other medications. However, it's still recommended to take D-Mannose at least two hours apart from any other medication or supplement.
D-Mannose* is suitable for preventive or supportive use in uncomplicated urinary tract infections and kidney stones during pregnancy and breastfeeding. However, it's recommended to consult a doctor before taking D-Mannose.
D-Mannose* can also be taken preventatively or as a supportive measure for bladder infections, such as cystitis, during pregnancy. It is advisable to have a prior consultation with your treating doctor/doctor beforehand.
D-Mannose* can also be used preventatively or to support the treatment of urinary tract infections or other uncomplicated urinary tract infections during breastfeeding. It is recommended to discuss this with your doctor beforehand.
D-Mannose* is hardly metabolised and therefore has no interactions with other substances. You can safely take D-Mannose* alongside antibiotics during acute bladder infection treatment.
Note: If your bacteria have mannose-sensitive fimbriae (e.g. E. coli, Klebsiella), D-Mannose* will often work so well that antibiotics are not necessary. What's important is that you take D-Mannose* preventatively, not just when the bladder infection is fully developed (the bacteria can settle in the bladder wall and hide).
D-Mannose* is effective in treating acute urinary tract infections and cystitis. It's just as good (if not better) for preventing recurring infections or to prevent the 'honeymoon cystitis' after sex. Condition: Your usual bacteria (please have this tested through a urine culture) has Type I-Pili, such as E. coli, Klebsiella spp., Serratia spp.
Even though you may only need a few days for effective treatment, there's no harm in taking it for longer. For D-Mannose*, there's no tolerance effect and no known resistance development.
There are many different instructions online, ranging from simple to complex. D-Mannose* is essentially impossible to overdose on. The worst side effect would be gastrointestinal discomfort (bloating, diarrhoea).
Therefore, my personal approach (as long as you don't get stomach pain): With acute bladder inflammation, take at least 2g per glass of water (about every 2-3 hours) min. 2g (or more, which you'll need to test yourself). Continue taking the dosage for a few days after symptoms have subsided and gradually reduce it.
For prevention of recurrent HWI, take morning and evening 2g. The most important thing is the evening intake, so that the D-Mannose* can work in the bladder during the night hours (it gives your bacteria no chance to multiply unchecked over several hours and establish themselves).
For bladder infections after sex: Take 1 glass of water with 2g (or more) D-Mannose* both before and after. If HWI keeps recurring even after sex: Increase the dose or have a urine culture done to find out which bacterium is responsible - maybe it's a mannose-resistant bacterium.
It varies from person to person. Some women (and men) report a improvement within a few hours. However, it can take longer depending on how far the bacteria have multiplied and spread. If there is no improvement after 3-5 days, it is advisable to visit a doctor's surgery.
In a study with 308 women, all of whom suffered from recurring urinary tract infections, the women received either 2g of D-mannose or 50mg of an antibiotic every day for half a year.
The result: Only 15% of the women in the D-mannose group experienced a recurrence, whereas 20% of the women in the antibiotic group did. The frequency of side effects was significantly lower in the D-mannose group compared to the antibiotic group.
It's only fair to note that the study was a comparison of the effectiveness of antibiotics versus D-mannose in preventing recurrence. If there is already an active infection, the result would likely be different. Therefore, it's essential to use D-mannose* primarily for preventive purposes.
If your D-Mannose* is not effective for a straightforward UTI, then there are at least two possible reasons. You may be dosing too low or you may have a naturally mannose-resistant bacteria (some strains of E. coli, Staphylococcus, Streptococcus, Proteus Mirabilis, etc.). If this is the case for you, then consider using other methods instead, such as Angocin Anti-Infekt N*.
Taking high doses of D-Mannose* can, in some cases, lead to digestive discomfort such as bloating, constipation and diarrhoea. If the digestive problems are manageable, it is best to persevere. Otherwise, you may try reducing the dose or fighting with other means, for example, with Angocin® Anti-Infekt N*.
Yes, D-mannose* from birch is also suitable for allergy sufferers.
The myth persists that D-mannose from maize is preferable in cases of birch pollen allergy. However, it is clear that D-mannose is a simple sugar and not a protein that can cause allergic reactions.
If you still feel like you are reacting allergically, please check your D-mannose* product. Is it simply pure D-mannose* or does it contain additional additives, such as cranberry, plantain root extract, pumpkin seeds? Is the powder produced by a certificate of good manufacturing practice (cGMP) compliant manufacturer?
As I'm not a doctor and being extremely cautious with children, I wouldn't recommend anything. You'll find both yes and no answers on the internet.
If I were to decide for my child personally, as D-mannose is simply a special form of sugar without additives - I would try D-mannose* (after consulting a doctor or nurse). The germ must be well-known and mannose-sensitive, and the dosage would need to be correspondingly lower. When choosing the preparation, I would put the highest emphasis on quality, origin and external laboratory tests.
As a child, I suffered from the dreadful pain of cystitis, so I understand how it feels for a child.
No, D-Mannose* and Birch Sugar are not the same.
Although D-Mannose* is present in blackcurrants, they contain much less active substance than pure D-Mannose powder. Pure and concentrated D-Mannose powder is therefore the better alternative and works 10-50 times stronger than blackcurrant juice.
Potential synergistic effect: Blackcurrant products also contain so-called proanthocyanidins, which prevent manganese-resistant fimbriae (type P fimbriae) from attaching to the urethra and bladder. D-Mannose* and the proanthocyanidins in blackcurrant extract could therefore be beneficial when combined.
Scientific studies are, however, moving on very thin ice when it comes to the effectiveness of cranberry products. A Cochrane meta-analysis (2012) which evaluated 24 studies with a total of 4475 participants found no evidence that cranberry products can prevent UTIs. If you still believe in the benefits of cranberry products and want to try them, it won't hurt to add D-Mannose* to your diet. Note: Blackcurrant capsules are preferable to blackcurrant juice, as the juice also contains a lot of sugar which can serve as food for most bacteria, promoting their growth and multiplication.
Forskolin
Coleus forskohlii, also known as Plectranthus barbatus, Indian Coleus or the Sanskrit name Makandi is a tropical plant, closely related to the Coleus species. Forskolin* is the active ingredient of the "Indian Painted Nettle" and also a food constituent from the group of terpenes, which are the main component of essential oils.
In China, India, Brazil and large parts of Africa, the active ingredient has been used in traditional medicine for centuries. In Western medicine, Forskolin* is used to treat Asthma, heart diseases and thrombosis. Forskolin extracts are also believed to aid weight loss.
Forskolin* is considered a blood pressure reducer (it dilates blood vessels) and anti-coagulant.
And now it gets interesting: It prevents the adhesion of bacteria to the bladder mucosa, which you can use to your advantage in fighting recurring urinary tract infections.
What researchers have found out about Forskolin in mice by instilling it into the bladder using Forskolin* could have a similar effect in humans. Forskolin interrupts the hiding game of bacteria embedded (E. coli) in the bladder wall. How does Forskolin do that? I'll need to take a bit of a detour and explain first, with what tactic bacteria can "nest" themselves in the urothelium.
The research team led by Brian Bishop from Durham University found out that the bacteria use a mechanism to remain in the bladder. In response to increasing urine flow rates, more cAMP (cyclic adenosine monophosphate) is produced within the endothelial cells of the bladder wall. This messenger substance causes small vesicles from the cell interior to move to the surface, where they fuse with the cell membrane and increase its size as the bladder expands. When cAMP levels drop after emptying the bladder, the vesicles are retracted and returned to the inner cell. And that's exactly when the pathogens slip into the vesicles and thereby gain access to the safe interior of the cells, where they are no longer affected by antibiotics.
Forskolin* counteracts the hiding game by increasing cAMP levels. As a result of increased cAMP levels, the small vesicles move to the surface again and embedded/buried bacteria gain access back into the bladder.
Studies have shown that the bacteria build a sort of biofilm. This film provides the pathogens with protection from antibiotic attack. This explains why some antibiotics are only temporarily successful. Sometimes, bacteria embedded in the bladder wall can break free after months and cause recurring bladder infections.
Hmm, although some reviews suggest it might be. Forskolin* is actually a promising treatment, which may help put an end to interstitial cystitis. However, using Forskolin alone is unlikely to provide any relief as it only pushes the bacteria out of their hiding places. To get rid of them for good, a 2nd step is needed to eliminate the bacteria in the bladder. This can be done through increased drinking and urination (flushing), combined with herbal supplements (*D-Mannose*, *Angocin Anti-Infekt N*, etc.) or antibiotics.
Conclusion: We don't know what a effective dose of Forskolin* is for humans and we have no evidence that Forskolin alone can cure bladder infections.
My Tip: Forskolin* has been around for centuries, indicating that it is safe. Try it out, perhaps it will be your breakthrough.
If your urine tract infection (UTI) is caused by bacteria with mannose-sensitive fimbriae (e.g. most E. coli strains, Klebsiella), they can be effectively targeted with D-Mannose*. The bacteria will then bind to the D-Mannose rather than the urinary tract lining, where they would normally cause inflammation or become trapped in vesicles. And precisely because of these bacterial hideaways, Forskolin* comes into play. Forskolin* brings the trapped bacteria back into the urinary tract, where the D-Mannose* then ensures that the E. coli bacteria cannot reattach themselves to the urinary tract lining. At the next urination, the neutralised sugar-bacteria complexes will be flushed out.
In an emergency: Total treatment duration of 10 days. Forskolin* 2 times a day (morning and evening), 400-500 mg Coleus Forskohlii extract with 20% concentration (equivalent to: 80-100 mg pure Forskolin). Mannose at least 6 times a day, 2-4 g, then gradually reduce the dose over a few days.
For prevention: Every few months for 1-2 weeks. Forskolin* 2 times a day (morning and evening), 400-500 mg Coleus Forskohlii extract with 20% concentration (equivalent to: 80-100 mg pure Forskolin). Mannose 2 times a day (morning and evening), 2-4 g. Note from experience reports: Forskolin* 1 hour before taking D-Mannose* (Tip: First, the bacteria must be lured out and then eliminated).
If the above treatment does not work or if you prefer a natural alternative, consider taking D-Mannose.
If you prefer to use a natural antibiotic, consider replacing D-Mannose with Angocin® Anti-Infekt N*.
Forskolin* 2 times a day (morning and evening), 400-500 mg Coleus Forskohlii Extract with 20% concentration (equivalent to: 80-100 mg pure Forskolin). Forskolin* 1 hour before taking D-Mannose* or other (natural) antibiotic remedies. Tip: First, the bacteria must be lured out with Forskolin, then Mannose or other remedies can make them harmless.
Yes, this is actually a very good idea as it helps the antibiotic to reach the pathogenic germs. As long as the embedded bacteria are hiding in the cells of the bladder lining, unfortunately, an antibiotic cannot do anything about it. It's only when the germs are sitting on or floating inside the bladder itself that they can be neutralised by a natural antibiotic.
Capsules containing Coleus Forskohlii extract are generally 100% natural, as the ingredients are of plant origin. In traditional Eastern medicine, the active ingredient has been used for centuries, which suggests a certain level of safety. However, other substances are often added - particularly to the capsule shell - and you should check this in the packaging instructions.
It's essential to look out for products that have undergone laboratory testing. You can identify safe products by checking if they meet international quality standards (HACCP, GMP), or adhere to an ISO standard.
Forskolin should not be taken during pregnancy and breastfeeding. As Forskolin has a blood-thinning and blood-pressure-lowering effect, it's not suitable for people with low blood pressure, taking medication for high blood pressure, those with clotting disorders or undergoing surgery.
Not just my favourite: Vitabay offers high-quality, vegan capsules with 80 mg pure Forskolin per capsule: Forskolin*.
There are no noteworthy or health-damaging side effects from taking Forskolin*. However, Forskolin can have a significant impact on blood pressure and circulation. Therefore, caution is advised in the following situations:
- If you have low blood pressure or are taking medication to control high blood pressure
- If you have bleeding disorders or are taking anticoagulant medications
- At least 2 weeks before surgery
- During pregnancy and breastfeeding
The experiences with Forskolin* are mostly positive. However, you should not expect an improvement after just a few days of taking it. As a preventative measure or for follow-up treatment after an acute infection, you can take it for several weeks and then every few months (provided you tolerate Forskolin well). The combination with a natural antibiotic (e.g. Angocin® Anti-Infekt N*) or D-Mannose* is definitely a good idea. Even together with antibiotics, it can be helpful. There are even reports of success stories in treating children, although no recommendation for using Forskolin on children has been made.
However, there are also some reports of intolerance, or that Forskolin has triggered more burning in the bladder/urethra. Some people report a flare (a recurrence of symptoms) after taking Forskolin. Others have reported no effect.
My tip: Just make your own experiences with Forskolin*! Stick to the recommended dosage and take it for a long enough period if you tolerate it well. Vitabay offers high-quality, vegan capsules with 80 mg pure Forskolin per capsule: Vitabay Forskolin
Vitabay offers high-quality, vegan capsules containing 80mg pure Forskolin per capsule: Forskolin*.
If you choose a different product, please make sure to read the ingredients and dosage carefully. Some products claim to contain 1000mg Coleus Forskohlii extract per tablet, but only 15mg of pure Forskolin is actually left. At a daily dose of 2 x 80mg, you would need to take at least 10 tablets per day.
Criticism about the products does exist, however. The capsules often contain fillers like magnesium carbonate. Generally speaking, they are considered safe by law as long as a certain daily dose is not exceeded. However, in higher doses (e.g. when taking many dietary supplements or medications containing this ingredient), magnesium carbonate can lower the absorption of other essential nutrients and cause bloating or diarrhoea.
Generally, the effect of Forskolin* is utilised by increasing cAMP levels, causing small vesicles to migrate from the cell interior to the surface and expelling encapsulated/pathogenic bacteria back into the bladder. The active ingredient Forskolin prevents the encapsulation of bacteria in the bladder mucosa.
At which fungal strains does Forskolin work now: Online, one usually finds this information only for E. coli. I would think that Forskolin works on all fungal strains that reside and hide in the bladder mucosa. My opinion therefore: It's worth trying Forskolin*, even if your fungus is not E. coli.
Very interesting, new findings:In an in-vitro study, the antibacterial and antifungal activity of plant extracts from Coleus forskohlii was investigated against some selected pathogens (Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae and Candida albicans). A strong antimicrobial activity against gram-positive and gram-negative bacteria was shown. The water extract of Coleus showed a maximum inhibition zone against Klebsiella pneumoniae, followed by Escherichia coli and Staphylococcus aureus. Even the fungus Candida albicans reacted sensitively to the strong antimicrobial activity of the Forskolin extract.
Chitosan* is available in retail as a weight loss aid. A long-chain sugar molecule derived from chitin (a fibre from shellfish), whose chemical composition is slightly altered, promises a similar effect to Forskolin*. Chitosan* acts as a bladder wall exfoliant: it removes the superficial layer of bladder cells, exposing hidden bacterial nests in deeper layers. Once the released bacteria are back in the bladder interior, they can be fought with antibiotics or natural remedies and flushed out.
So far, this phenomenon has been observed in studies with mice injected with bacteria and then Chitosan* in their bladder. When UPEC (uropathogenic E. coli) infected mice are given Chitosan* and antibiotics on several consecutive days, the mice are cured. However, evidence of its effectiveness in humans is still lacking.
Interactions and side effects of Chitosan: Chitosan* not only binds cholesterol and "fat-inducing" fats. It also causes the body to excrete valuable fat-soluble vitamins such as vitamins A, D, E, and K or essential fatty acids alongside the fat blocker. Medications such as contraceptive pills, blood thinners, or antiepileptics are also bound by Chitosan, are not absorbed in the intestines, and do not enter the bloodstream to take effect. As a countermeasure, manufacturers recommend taking fat-soluble vitamins and medications at least four hours before or after Chitosan. However, it is not yet definitively proven whether this is sufficient. Whether Chitosan can be safely taken orally in high doses has not been confirmed by the consumer protection agency. People allergic to crustaceans and shellfish should avoid Chitosan. It is also unclear whether oral intake of Chitosan leads to a similar concentration in the bladder.
What would I do? If I could not tolerate Forskolin* and were struggling with recurring UTIs, I would definitely try Chitosan. I have known this remedy for more than two decades – I originally bought it as a "fat blocker."
Forskolin* has a blood pressure-lowering and blood-thinning effect, so there are interactions with the following medications: antihypertensive drugs, blood thinners.
Chitosan* binds not only fats, but also other active substances: anti-pregnancy pills, blood thinners, antiepileptics, fat-soluble vitamins (Vitamin A, D, E and K). As a countermeasure, manufacturers recommend taking fat-soluble vitamins and medications at least four hours before or after Chitosan. Whether this is sufficient is still not finally clarified.
My conclusion: There are no direct interactions between Forskolin and Chitosan. However, Forskolin is a fat-soluble substance and fat-soluble means that the active substance does not dissolve in water but in fats.
Natural Antibiotics
Although most conventional antibiotics also originate from nature (the major antibiotic classes were discovered in soil organisms), this question usually refers to something else.
The following natural antibiotic substances can be helpful in treating problems in the urogenital tract (uncomplicated UTIs, vaginal yeast infections, bacterial vaginosis, etc.):
- Horseradish and nasturtium (sulfides, mustard oil glycosides)
- Ginger, turmeric (terpenes)
- Olive leaf extract and uva ursi (polyphenols)
- Oregano oil* (terpenes and phenols)
- Piperine from black pepper (alkaloids)
- Garlic* (sulfides, allicin)
- Apple cider vinegar, honey, chamomile
There are really good alternatives to antibiotics, which, although they do not have exactly the same mechanism of action, lead to the same goal: Goodbye UTI!
Here is a list of alternatives:
- Phytopharmaceutical #1: Angocin® Anti-Infekt N* (nasturtium herb and horseradish root) acts through the antimicrobial mustard oil glycosides it contains. Numerous studies support the pronounced germ-inhibiting effect of isothiocyanates (ITCs, mustard oils). The growth of multi-resistant germs and even the formation of resistant biofilms can be inhibited.
- Phytopharmaceutical #2: Canephron®* (centaury, lovage root, rosemary leaves) showed comparable effects to the antibiotic fosfomycin in a larger study.
- More from nature: The allicin in fresh garlic has antibacterial and antifungal properties. Besides garlic, there are many other foods that act similarly to antibiotics; see Where can antibiotics be found in nature?
- D-Mannose: In a controlled study, daily intake of 2g D-Mannose* proved as effective as long-term antibiotic prophylaxis (over six months) with 50mg nitrofurantoin daily.
- Antiseptic: English scientists showed in a study that taking the antiseptic methenamine can prevent infections as effectively as antibiotics. Since its antiseptic action is based on the release of potentially carcinogenic formaldehyde in the urine, this substance is not available in DACH. However, the medication can be purchased online, e.g. in Denmark (trade name Haiprex®) or England (trade name Hiprex®).
- Vitamin C: High-dose vitamin C therapy administered intravenously is an alternative to antibiotic treatment and often the only effective approach for chronic infections. Numerous in vitro studies demonstrate the effectiveness of vitamin C (ascorbic acid) in inhibiting germs (even gram-negative bacteria like K. pneumoniae, E. coli, P. aeruginosa, P. mirabilis). While there are few in vivo studies, many women have reported eliminating Staphylococci and Enterococci (gram-positive bacteria) by taking high-dose oral vitamin C (3-4 times daily, 3g ascorbic acid).
There are many effective substances from the plant world that work in a similar way to antibiotics. However, it's not possible to give a blanket answer as to which one is the best natural antibiotic. If you know which germ is causing the problem, then you can take a more targeted approach and tackle it on multiple fronts naturally.
To find substances with a similar effect to antibiotics, see What has the same effect as antibiotics?
Generally speaking: D-Mannose* for E. coli or Klebsiellen, Angocin Anti-Infekt N* for almost all germs, for gram-positive bacteria (Staphylokokken, Enterococcus faecalis) acidification with Vitamin C.
In the article Infection Compass, you'll find more information about which natural remedies are best for various germs.
You can find foods that have a similar effect to antibiotics under What has the same effect as antibiotics?, and Where can I find antibiotics in nature?
If you're looking for a list of plant-based substances found in supplements, you might find it in an article from the "German Pharmacist's Journal": Plant-based substances in supplements
Grapefruit seed extract (often abbreviated as GKE / GSE / GFSE), discovered by Dr. Harich in 1970, has gained significant popularity as a dietary supplement. Grapefruit extract is said to have antifungal and antibacterial properties, meaning it supposedly inhibits the growth of bacteria, viruses, and fungi.
I have heard from some fellow sufferers who swear by the effectiveness of high doses of GKE to fend off a developing bladder infection. However, no scientific evidence has yet been found to support the alleged universal efficacy of GKE.
The data is therefore sparse. A 2013 study also indicates that it is still unknown whether grapefruit seed extract is effective in humans or even safe.
Other studies suggest that the "miraculous" effects of GKE are likely due to preservatives such as benzethonium chloride, triclosan, and methylparaben present in the extracts. These studies have proven the presence of such preservatives in grapefruit seed extract. For this reason, the Federal Institute for Risk Assessment warns against the dietary supplement grapefruit seed extract.
Benzethonium chloride, for example, is not approved for use in food. Even cosmetics are allowed to contain only 0.1 percent of it. It is alarming that some grapefruit seed extract products have been found to contain more than 10 percent benzethonium chloride.
Benzethonium chloride is a substance with antimicrobial properties that likely does not occur naturally in grapefruit seeds and was presumably added unlawfully.
Another piece of evidence that the efficacy of GKE is due to the preservatives in the extract: Pure grapefruit seed extract without additives showed no effects. The ineffective extract (CitroBiotic) is reportedly made from a base concentrate free of preservatives and pesticide residues, unlike the imported U.S. extract.
Focusing on the bladder: Only 0.5 percent of the absorbed dose (quercetin and its metabolites) is excreted in the urine. This raises the question of how substances can still be effective under such unfavorable conditions. To date, science has not provided conclusive proof of effectiveness.
Warning: Side effects/interactions: Grapefruit seed extracts are often classified as harmless dietary supplements. However, a case from the U.S. shows that taking the antihistamine terfenadine with two glasses of grapefruit juice can have fatal consequences. Those taking medications such as nifedipine, felodipine (blood pressure drugs), or warfarin (blood thinners) should avoid grapefruit and always consult a pharmacist.
According to the Gelbe Liste, grapefruit juice interacts with a wide range of medications, and GKE is contraindicated for those with citrus allergies.
Apart from the preservatives in the extracts, grapefruit seeds contain numerous bioflavonoids. Flavonoids are known for their diverse pharmacological effects and are used in a wide range of therapeutic applications: antioxidative, cardiovascular-stimulating, anti-inflammatory, capillary-sealing, edema-protective, platelet aggregation-inhibiting, antiparasitic, and cancer-protective.
These secondary plant compounds found in grapefruit seed extract are currently an exciting topic in research due to their cell-protective properties, which may help protect against numerous diseases. However, you don't need a dietary supplement like grapefruit seed extract to access these compounds: A balanced diet rich in seasonal vegetables and fruits can provide you with antioxidants and many other essential nutrients just as effectively.
My conclusion: A fellow sufferer reported the healing effects of high doses of GKE for urinary tract infections, but paradoxically, it had to be the original by Dr. Harich. It’s important to note that Dr. Harich’s GKE product was one of those found to contain the aforementioned harmful preservatives, which could explain why this extract "works." Before researching this dietary supplement, I also believed it was entirely health-promoting. However, this does not appear to be the case. Even worse, it may actually be harmful to health. Only products without the dangerous preservatives (e.g. CitroBiotic) are not harmful. Therefore, my advice: Please exercise caution with this "miracle remedy."
In the case of a severe bacterial urinary tract infection, your doctor will likely rely on conventional treatment with antibiotics. For mild infections, such as an uncomplicated bladder infection (especially in the early stages), plant-based medicines, known as phytopharmaceuticals, are a genuine alternative to classical antibiotics.
Here is a list of benefits when using natural AB:
- Effectiveness against viruses and fungi (synthetic AB only work against bacteria)
- No or very few side effects (synthetic AB can cause issues such as digestive problems, rashes, cystitis, and often weaken the gut flora)
- No resistance development against the plant-based ingredients (overuse and/or misuse of synthetic AB leads to resistance formation)
Despite all these advantages, plant-based medicines will not be able to replace traditional antibiotics. With natural remedies, patience is required: while conventional ABs show quick results, you may only notice the effects of natural remedies after longer use.
Unfortunately, this question cannot be answered definitively. Plant-based antibiotics can work differently well, depending on the type of bacteria you're dealing with.
If you want to know exactly which Natural Antibiotics will best help your infection, then you'll need to have a so-called Aromatogram done.
You can find more information under What is the best natural antibiotic?
An Aromatogram is comparable to an Antibigram. A disc diffusion test (in-vitro test) indicates the susceptibility of the previously isolated pathogen to various essential oils. The larger the resulting zone of inhibition, the more effective the individual essential oil.
Depending on the results of the Aromatogram, individual "aromatherapeutic" medicines are then prepared from the active essential oils in an aromatherapy-qualified pharmacy. You receive a kind of your own pathogen-specific blend for aromatherapeutic treatment of e.g. vaginal and urinary tract infections.
When performing an Aromatogram, a variety of essential oils are tested: lavender, eucalyptus, thyme, lemongrass, neroli, manuka, tea tree, rose geranium, etc.
Angocin Anti-Infekt N* contains the active ingredients Capsicum powder and Radish root powder. The constituents of both plants act against Bacteria, Viruses, Fungi as well as stimulating and supporting the immune system. Angocin Anti-Infekt N* is often used for complaints of acute inflammatory diseases of the bronchi, sinuses and urinary tract.
Angocin Anti-Infekt N* is not a traditional, synthetic antibiotic. The capers and horse radish in Angocin contain so-called mustard glycosides with threefold effect: against bacteria, against viruses and against inflammation. Various studies prove the tolerance and efficacy of the plant mustard glycosides. In comparison to conventional antibiotics, no resistances have been observed yet.
Numerous clinical studies confirm the antibacterial effectiveness of dandelion and horseradish in sinusitis, bronchitis or cystitis. In cases of mild to moderate infections, treatment with dandelion and horseradish extracts is as effective as conventional antibiotics.
A study at the University Hospital Freiburg found that saponin glycosides from dandelion root and horseradish root have a pronounced inhibitory effect against 13 types of bacteria, including MRSA, a problem bacterium.
How does Angocin work? After swallowing the tablets, they are broken down in the stomach and the conversion process of saponin glycosides is initiated. The saponins are then quickly and completely absorbed in the upper part of the small intestine, entering the bloodstream. From there, they eventually reach their excretory organs, the bladder and lungs, where they exert their antibacterial effect exactly at the site of infection.
The recommended dose is: 3-5 times a day, take 4-5 film tablets each time Angocin® Anti-Infekt N*. In the case of an acute infection, take the maximum dose (5 times a day, 5 tablets) each time.
The most tolerable way is to take the medicine after meals, as Senföle can cause stomach and intestinal discomfort.
If you're experiencing stomach and digestive issues, try taking Angocin Anti-Infekt N* consistently after meals (never on an empty stomach). If you still can't tolerate Angocin, you may want to consider alternative natural antibiotics. See Where can I find antibiotics in nature?
Angocin® Anti-Infekt N* must not be taken if any of the following applies:
- Acute stomach and bowel ulcers
- Acute kidney inflammation
- Allergy to dandelion root, burdock root
- Under the age of 6 years old
Only take after consulting your doctor if any of the following applies:
- Pregnancy and breastfeeding
- When taking anticoagulant medications
- Between the ages of 6 to 12 years old
I am generally very cautious when using the term "wonder cure", but nasturtium and horseradish are indeed very effective medicinal plants.
Many commercially available plant-based supplements lack scientific evidence (which, to be fair, can also not always be easily proven for phytopharmaceuticals). However, the glucosinolates from nasturtium and horseradish have been scientifically proven multiple times to be effective and safe. A study analysis of more than 30 research papers published between 2000 and 2019 confirms: Glucosinolates from nasturtium and horseradish possess a well-documented antibacterial and anti-inflammatory effect profile, making it difficult for bacteria to adhere to bladder lining cells, and can even inhibit the formation of biofilms.
The large-flowered nasturtium was chosen by scientists at the University of Würzburg as the Medicinal Plant of the Year 2013.
The authors of the current S3 Guideline for the treatment of "uncomplicated urinary tract infections" recommend using plant-based medication with nasturtium and horseradish as a natural treatment option in cases of recurring bladder inflammation.
Do you suffer from an acute, uncomplicated urinary tract infection? Then, taking the maximum dose (five times daily, five tablets) should result in a noticeable improvement within a few days.
To prevent recurring infections, Angocin Anti-Infekt N* can be taken prophylactically at the standard dose (four film tablets three times daily) for an unlimited period.
Red clover and horseradish are really effective, natural antibiotics. However, there are some bacteria that show less sensitivity to the mustard seeds - namely Enterococcus faecalis and Enterococcus faecium.
If Angocin Anti-Infekt N* is not helping you, you can opt for many other natural antibiotics: see Where can one find antibiotics in nature?.
Sometimes it's also the case that you won't get rid of your bacteria (or mixed infection) without synthetic antibiotics. In such cases, a urine culture with antibiogram is absolutely necessary to determine which antibiotic is sensitive at your bacteria / your bacteria.
Acute: As soon as you notice a bladder inflammation starting, full dose: take 5 tablets five times a day, ideally after meals. Do this for at least 5 days.
Follow-up / Prophylaxis: After around 5-7 days of maximum dosage, you can reduce the dose: take 4 tablets three times a day (unlimited duration if well tolerated)
The package insert does not restrict the duration of administration. So, if Angocin Anti-Infekt N* helps you, you can continue to take it as long as you find it beneficial.
My tip: If you have overcome a BE with Angocin, I recommend a prophylactic intake of the standard dose over a period of 1-2 months. 1-2 months are the time frame in which bladder inflammations tend to recur. Do you experience HWI after sex? Then I recommend taking the maximum dosage for a few days afterwards.
According to the manufacturer, there are no known interactions between Angocin® Anti-Infekt N* and Antibiotics. This means there are no concerns when taking ANGOCIN Anti-Infekt N and classical antibiotics at the same time.
My opinion: Since dandelion root and garlic have the potential to inhibit biofilms, I believe it's a good idea to combine Angocin and Antibiotics as most synthetic antibiotics are only partially effective against biofilm-adherent bacteria.
The medication is generally well-tolerated, but I've heard from fellow sufferers that some people experience stomach and bowel problems more frequently. According to the packaging insert, the following side effects have been reported:
- Frequently (max. 1 in 10): Nausea, upper abdominal discomfort, diarrhoea, bloating or heartburn
- Allergic reactions such as skin redness, rashes, itching
If you experience stomach and bowel problems, please check again that you've taken the tablets after meals and not on an empty stomach. You can also try reducing the dose to see if it alleviates the side effects.
In cases of allergic reactions, please discontinue use. You can explore alternative options, see Where can I find antibiotics in nature?.
Not only various studies demonstrate the effectiveness of mustard and horseradish. I also regularly read in forums and Facebook groups that Angocin® Anti-Infekt N* has helped many people, to get recurring bladder infections under control.
If you'd like to do some research yourself, simply read customer reviews on online shops that sell Angocin® Anti-Infekt N*, such as Amazon or Boots.
Or you can join a search and exchange with people who are suffering, such as the facebook support group Bladder Infection - Help, Support & Exchange
The most well-known variety is probably Angocin® Anti-Infekt N*, which contains high-dose mustard oils from cress plant and horseradish root.
Even higher dosed are the Horseradish-Cress Capsules by the German company GEKO - Fa. Wolfram Medenbach.
There are other products on the market that I haven't tested myself yet. In this case, I would recommend paying attention to origin, certification mark and ingredients.
All preparations are available over-the-counter in pharmacies or online.
The University Hospital of Freiburg has determined the so-called MHK90 for 13 different pathogens, which indicates that at least 90% of the tested strains of a species were completely eliminated by the active substance combination (= no growth on the test plate).
For example, with Angocin® Anti-Infekt N* (1 tablet contains 200mg of caper plant powder and 80mg of horseradish root powder), the following number of tablets was required to eliminate 90% of the tested bacterial strains.
Gram-positive bacteria:
- Staphylococcus aureus (MSSA): 2 tablets
- Pathogenic Streptococci: 5 tablets
- Enterococcus faecalis, Enterococcus faecium: more than 6 tablets
Gram-negative bacteria:
- Pseudomonas aeruginosa: 2 tablets
- Escherichia coli: 2 tablets
- Proteus vulgaris (note: not Proteus mirabilis, which is a different species): 2 tablets
Pain Relief
You probably belong to the sisters who, with an acute cystitis, suffer from hellish pain. Every trip to the loo is a torment when you have cystitis!
On the one hand, the terrible pain when emptying the bladder, on the other hand, the constant and nagging ache that won't let up. Especially nights are still vivid in my memory.
While the statement "Today no one should have to suffer from pain" may not be entirely accurate - but painkillers can certainly help alleviate your torment with cystitis. Even the current S3 guideline speaks out in favor of Ibuprofen alongside antibiotics and phytopharmaca (plant-based medicines). For Ibuprofen, see
A study compared the effect of primary symptom-based treatment with Ibuprofen to immediate antibiotic treatment. Under Ibuprofen, 70% of patients were free from symptoms after one week (80% in the case of antibiotic treatment).
Diclofenac was also looked at: After three days, 54% in the Diclofenac group versus 80% in the Norfloxacin group were free from symptoms (83% vs. 96% after seven days).
Warning! Painkillers can mask a critical course: In a purely symptom-based treatment with Ibuprofen (or Diclofenac etc.), there is still a 5% risk of pyelonephritis. This means for you in plain English: painkillers yes, but don't overdo it. Pyelonephritis signals itself through fever, flank pain, discomfort, chills. Then by no means increase the Ibuprofen dose, but go to your doctor for antibiotic treatment!
The largest group of over-the-counter painkillers are non-steroidal anti-inflammatory drugs (NSAIDs), such as Ibuprofen and Diclofenac. Another commonly used over-the-counter painkiller is Paracetamol. It also has pain-relieving and fever-reducing effects, but unlike NSAIDs, it does not have anti-inflammatory (anti-phlogistic) properties. Without a prescription, you can buy the following in the pharmacy:
- Ibuprofen: up to 400 mg per tablet (e.g. IBU-ratiopharm®, NUROFEN®)
- Diclofenac: up to 25 mg per tablet (e.g. Voltaren®, Diclo-ratiopharm®)
- Paracetamol: up to 500 mg per tablet (e.g. Paracetamol-ratiopharm®)
Also effective (but prescription-only) is the active ingredient
- Metamizole: up to 500 mg per tablet/drop (e.g. Novaminsulfon®, Novalgin®)
Metamizole is an analgesic with weak anti-inflammatory effects. Compared to NSAIDs (like Ibuprofen), Metamizole has an overall at least comparable, possibly even better, benefit-risk profile. Especially interesting for those with kidney problems: Unlike NSAIDs, Metamizole has minimal impact on kidney function.
A short-term use of over-the-counter painkillers rarely leads to serious side effects. However, you should please be cautious if the following applies to you: you are over 65, you have stomach or bowel conditions, you are taking anticoagulants, you have had a heart attack or stroke, you have high blood pressure, or you have kidney issues. Please read the package insert before taking!
Cramps
If you suffer from cramps (sometimes following an acute urinary tract infection), in addition to painkillers, so-called spasmolytics can help. Spasmolytics such as Buscopan®* (Butylscopolamine), Spasuret®* (Flavoxat) and others relax the bladder muscles. Buscopan® PLUS additionally contains Paracetamol as a painkiller.
Spasmolytics, especially anticholinergic substances like Butylscopolamine, are not free from undesirable side effects (e.g. dry mouth, constipation, and palpitations). Please read the package insert before taking anything. Unlike other substances used for this purpose, Flavoxat (brand name Spasuret®*) is not anticholinergic.
Urinary tract infection versus overactive bladder: For an overactive bladder (sometimes also called urge or irritative bladder), prescription anticholinergics (=Parasympatholytics) are often used to suppress the symptoms. Anticholinergics block the action of the body's neurotransmitter Acetylcholine, which transmits nerve impulses in the nervous system. Examples of drugs are Spasmex®, Spasmolyt® (prescription-only). An overactive bladder must be diagnosed by a urologist after ruling out other conditions (e.g. acute/chronic urinary tract infection, oestrogen deficiency, completed bladder journal, emptying disorders, bladder cancer).
It is important to always choose the correct dose and not take painkillers for longer than necessary. If you prefer not to rely on chemicals, you can also read here: Which natural painkillers help with urinary tract infections?
If you'd like to avoid or can't take chemical painkillers, I would recommend the following:
- Heat & Relaxation: My tip: Try lying down with a hot water bottle or heating pad! Heat has a calming effect and can help ease tense or crampy lower abdominal pain.
- Soda Ash* against burning: I haven't tried it myself, but dissolving 1/4 teaspoon of baking soda (sodium hydrogen carbonate) in water and drinking it may help ease the burning sensation. This solution neutralises the acidity in the bladder and can alleviate the stinging pain caused by an acute UTI.
- Acupressure Mat*: Simply give it a try! It can help ease the pain in your bladder and also strengthen the bladder meridian. Stand on the mat with your feet shoulder-width apart, and slowly step back while applying gentle pressure.
Which pain relief has the strongest effect, cannot be answered generally. It depends on various factors such as dosage, form of administration and individual susceptibility. It also depends on the type of pain. For cramp-like pains, Buscopan(R) (Butylscopolamine) is often recommended. For general pains in the lower abdomen, lighter pain relievers like ibuprofen or paracetamol are usually given. Urologists also prescribe the prescription-only Novalgin(R) (Metamizol).
Not everyone responds well to one and the same pain relief.
That's why here are my personal tips:
- Ibuprofen: Unlike paracetamol, ibuprofen is also anti-inflammatory (antiphlogistic). The first choice of medication when possible (note: interactions with antibiotics of the fluoroquinolone group => always check the package insert!)
- Metamizol: Prescription-only (e.g. Novalgin(R)), but for that reason a few plus points: Users report a better pain-relieving effect, less straining on the kidneys, no interactions with the usual antibiotics for urinary tract infections, cramp-relieving. Therefore the second choice of medication when possible (always check the package insert!)
- Cramp relievers: If the first two pain relievers don't help, you can still try Buscopan PLUS(R) (also contains paracetamol) or Spasuret(R)* (less side effects on the central nervous system than Buscopan(R)).
For more information about some other pain relievers, see What pain relievers help with cystitis?
Heat, Rest & relaxation, anti-inflammatory painkillers like Ibuprofen or Metamizol (Novalgin), muscle relaxant painkillers like Buscopan PLUS or Spasuret. More information can be found under What painkillers help with cystitis? and Which natural painkillers help with cystitis?
Heat and painkillers like Ibuprofen or Metamizol (Novalgin), muscle-relaxing painkillers like Buscopan PLUS or Spasuret. More on this at Which painkillers help with cystitis? and Which natural painkillers help with cystitis?
What to do? The agonizing pains from acute cystitis are barely bearable! 1 tablet of Ibuprofen with 400mg doesn't help me at all when I take it before going to bed (or when I wake up at night due to cystitis). I take the maximum single dose of 2 tablets, each 400mg. Together with natural antibiotics like e.g. Angocin Anti-Infekt N or D-Mannose allows me to sleep further and the herbal medicines can work well in my bladder.
Taking both antibiotics and pain relief can lead to unwanted interactions, such as affecting kidney or liver function, or causing seizures. In any doubt, please read the packaging insert carefully for your specific antibiotic product, which should list all possible interactions. Alternatively, consult a doctor or pharmacist for advice.
There are no reported interactions with: The following antibiotics are listed as having no interactions with Ibuprofen:
- Amoxicillin
- Fosfomycin
- Nitrofurantoin
- Nitroxolin
- Cotrimoxazol
- Cephalosporine and Cefixim (Infectocef, Suprax, Cefastad, Cefaclor)
- Pivmecillinam (Selexid, Pivmelam, X-Systo)
- Trimethoprim (Infectotrimet)
Warning: Antibiotics in the Fluorochinolone group, such as Levofloxacin (e.g. Tavanic), Moxifloxacin (e.g. Avalox), Norfloxacin, and Ciprofloxacin can cause seizures when taken with anti-inflammatory medications like Diclofenac or Ibuprofen. Instead, consider using Metamizol (Novalgin) for these combinations, as there are no reported interactions. More information available here:
In my personal experience, when using antibiotics for UTIs and other infections: - If I need to take pain relief medication, I opt not to use it. - If I choose to take pain relief with antibiotics, I carefully monitor the effectiveness of the antibiotic treatment.
Opioid analgesics are substances with a morphine-like effect. In addition to the desired pain-relieving (analgesic) effect, these painkillers also have numerous other unwanted side effects due to binding at opioid receptors. Furthermore, two additional issues arise: tolerance development (you need increasingly higher doses to achieve the same effect) and withdrawal symptoms (opioids become addictive).
Well-known representatives from the list of opioid analgesics are: Tramadol, Tilidin, Morphine, Oxycodone (ranking according to analgesic potency)
Warning: The use of opioid analgesics must be justified by a doctor. Even if you have such medication at home or have access to it in some way: do not take them lightly with a urinary tract infection! The health cost-benefit calculation is certainly not favourable here. Moreover, strong painkillers could mask a kidney inflammation (pyelonephritis).
If you have cystitis and are experiencing pain, then opt for these medications instead: What painkillers help with cystitis?
Tramadol, Tilidin, Morphine, OxyContin and similar are strong painkillers from the category of opioid analgesics. More on this under What strong painkillers help with cystitis?.
If you have cystitis and are experiencing pain, it's best to opt for these remedies: Which painkillers help with cystitis?
Spasmolytics have smooth muscle relaxant properties affecting the urogenital tract. Neurotropic spasmolytics (= parasympatholytics) raise their anticholinergic effects on a portion of the autonomic nervous system. More precisely, anticholinergics inhibit the effects of the body's neurotransmitter acetylcholine, which transmits nerve impulses in the nervous system. This is done by a substance such as trospium chloride, for example, with trade names like Spasmex, Spasmolyt (prescription only), or the non-prescription available Buscopan (butylscopolamine).
Spasmolytics are often used in the treatment of an overactive bladder ("irritable bladder" or "spastic bladder"). Again, it is essential to note that OAB must be diagnosed by a urologist. In cases where there are uncomplicated urinary frequency issues, caution should also be exercised when taking spasmolytics, as they can also affect the emptying of the bladder. Urinary retention is not desirable in cases of bladder inflammation.
The topic of an overactive bladder alone could fill whole books. As my website focuses on the subject of bladder inflammation, I will not go into too much detail here.
My experiences:
- Self-diagnosis of overactive bladder: I often read that fellow sufferers quickly speak of an overactive bladder. A irritated bladder is not OAB (overactive bladder) and does not require treatment for OAB. An OAB must be diagnosed by a urologist/urogynaecologist and treated accordingly.
- Diagnosis of overactive bladder: Overactive bladder or mistaken chronic urinary tract infection? Sometimes the suspicion arises from experience reports that overactive bladder is diagnosed when therapists are at a loss for words. Often, therapeutic measures for overactive bladder do not work because it is actually an embedded bladder inflammation (which is even harder to diagnose and treat).
-
Treatment:
Among the therapeutic options are not only bladder medications. Rather, a form of step-by-step therapy is worked with:
- Behavioural changes, bladder training
- Pubococcygeus muscle training
- Bladder-regulating medications, e.g. Spasuret®*, Spasmex
- Electrical neuromodulation
- Botox injections into the bladder muscle
- Implantable electrical bladder pacemaker
- Surgical enlargement of the bladder
Spasuret* and Spasmex belong to the group of anticholinergics. These are substances that inhibit the bladder and prevent muscle tension.
This relaxes the bladder and frees those plagued by the overactive urge to empty the bladder from this problem.
What you should know when taking anticholinergics:
- Be patient! The effect will only take place after 2-4 weeks.
- Not just the bladder is dampened! Other organs that are regulated by the parasympathetic nervous system will also be suppressed. This can lead to dry mouth, constipation, palpitations, visual disturbances.
- High dropout rate - 40-80% discontinue use within the first 30 days
- Anticholinergics have a central effect on cognitive function.
How can unwanted side effects be avoided?
- No oral intake, but apply as a transdermal patch on the skin, e.g. Oxybutynin patch Kentera®
- Do not suppress the parasympathetic nervous system, but rather strengthen the sympathetic nervous system, e.g. Mirabegron (Betmiga®)
- Administer the medication directly into the bladder using a very small catheter (intravesical application), e.g. intravesical Oxybutynin solution (Vesoxx®)
- Herbal alternatives: e.g. Urox® a preparation from China (Tolterodine)
Antibiotics are very effective at killing bacteria in the urine, and for a long time they were the go-to treatment for cystitis. Unfortunately, there is now a growing number of bacteria that are resistant to a range of antibiotics. And despite this, doctors often prescribe an antibiotic unnecessarily.
The more frequently uncomplicated urinary tract infections are treated with antibiotics, the higher the risk of bacterial resistance to these antibiotics.
In other words: The more often you take antibiotics for cystitis, the more strains will eventually become resistant to them.
Antibiotic resistance is a global challenge - which is why a study published in 2015 compared Ibuprofen and antibiotics for treating uncomplicated cystitis. The result was: Around two-thirds of the 494 patients were also cured without antibiotics - a symptomatic treatment with the anti-inflammatory painkiller Ibuprofen was sufficient. In every third case, however, a classical treatment with an antibiotic was ultimately necessary.
Which means for you: As an otherwise healthy woman with mild to moderate symptoms, symptomatic treatment with Ibuprofen is often sufficient.
However, during the last three months of pregnancy (the third trimester), Ibuprofen (or Diclofenac) should not be taken.
More information can be found under Which painkillers help with cystitis? and Which natural painkillers help with cystitis?
Paracetamol is a over-the-counter and widely used, popular pain relief medication. Paracetamol relieves pain and reduces fever, but unlike NSAIDs (such as Ibuprofen and Diclofenac), it has no anti-inflammatory effect. As the bladder wall is inflamed in an acute cystitis, anti-inflammatory painkillers like Ibuprofen and Diclofenac have a double effect. They relieve the pain and also reduce inflammation.
In mild cases of pain, Paracetamol is the preferred option. If you experience stronger pain, I would recommend NSAIDs such as Ibuprofen or Diclofenac, provided that their use is suitable for you according to the packaging instructions. If you are not able to take NSAIDs, then a prescription-only painkiller like Metamizol (e.g. Novalgin) would be more effective than Paracetamol.
Useful to know: In mild cases of pain, you can take Paracetamol during the entire pregnancy.
Warning: Taking high doses of Paracetamol can be harmful to your liver. Therefore, it is recommended that you avoid consuming alcohol while taking this medication.
Phenazopyridine is a painkiller used to relieve symptoms associated with urinary tract irritation. It is available under the following brand names: Azo Standard, Pyridium, Prodium, Pyridiate, Baridium, Uricalm, Urodine, UTI Relief.
How does Pyridium work?
Phenazopyridine is used as an adjunctive medication for the treatment of symptoms related to urinary tract infections. Also known as a urinary analgesic, it relieves burning, urgency, frequency, and pain. However, Phenazopyridine is not an antibiotic and does not have bactericidal or bacteriostatic effects.
Paracetamol is a freely available painkiller. It works to reduce pain and lower fever, but unlike NSAIDs (non-steroidal anti-inflammatory drugs) it has no anti-inflammatory effect. Ibuprofen and Diclofenac belong to the group of NSAIDs and have an additional anti-inflammatory effect.
Paracetamol may be well tolerated, but is relatively ineffective => If you can take Ibuprofen or Diclofenac, I would recommend these painkillers over Paracetamol.
For more information on painkillers for cystitis, see our FAQs Which painkillers help with cystitis? and What are some natural painkillers for cystitis?
Both painkillers are non-opioid painkillers. The difference is that Ibuprofen belongs to NSAIDs (non-steroidal anti-inflammatory drugs) with anti-inflammatory properties, while Metamizole (e.g. Novalgin®) and Paracetamol are painkillers without significant anti-inflammatory effects.
Since a bladder infection is, as the name suggests, an inflammation, a painkiller with anti-inflammatory effects like Ibuprofen has a positive side effect in addition to its pain-relieving properties.
The prescription-only Metamizole is only barely to weakly anti-inflammatory, but is usually gentler on the stomach and kidneys. Furthermore, the pain-relieving effect of Metamizole is often stronger (although the effectiveness of a painkiller always depends on the dosage, form of administration, and individual susceptibility).
A very good article on the topic of various painkillers was published in the Swiss Medical Forum in 2017: Metamizole: Benefits and Risks Compared to Paracetamol and NSAIDs
More on the topic of painkillers for bladder infections can be found under Which painkillers help with bladder infections? and Which natural painkillers help with bladder infections?
Metamizol is an effective analgesic (= pain-relieving or pain-reducing medication) with weak anti-inflammatory effects. Metamizol is often prescribed as it causes fewer gastrointestinal side effects compared to other analgetics. Due to the severe side effect of agranulocytosis it is subject to a prescription requirement. Estimates of the incidence of agranulocytosis range from 1:1500 to fewer than one case per million applications.
Interesting summary:
- Clear advantages over NSAIDs (Ibuprofen and Diclofenac) if you have kidney failure or the risk of gastrointestinal bleeding.
- You will need a prescription from your doctor for Metamizol.
- Metamizol has a rare but severe side effect: agranulocytosis.
- According to experience reports, the dropper form works better.
- Metamizol is also spasmolytic, which can be helpful during cystitis.
- During the entire pregnancy, you should avoid taking Metamizol. In the third trimester, i.e. during the last three months of a pregnancy, Metamizol must not be taken.
You can find more information on pain relief medications for cystitis under Which pain-relieving medications help with cystitis? and Which natural pain relief medications help with cystitis?
Buscopan belongs to the group of medicines known as spasmolytics and is used, among other things, for spasmodic pain in the urinary tract. Buscpan PLUS is a pain tablet with dual action. It contains not only the spasm-relieving painkiller butylscopolamine, but also the pain-relieving substance paracetamol. With the same aim: to alleviate cramps and pain in the abdomen.
The active ingredient Butylscopolamin belongs to the anticholinergics, i.e. it affects the nervous system by blocking certain stimuli. Paracetamol blocks the production of prostaglandins, which are substances that play a significant role in the development of pain, fever and inflammation.
Buscpan PLUS relieves pain and resolves cramps in the abdomen for an acute, uncomplicated bladder infection. Reading experience reports from fellow sufferers shows very mixed opinions. For some, it's their go-to medication, while others report barely noticeable relief of symptoms.
Tolerance and analgesic efficacy are individual matters and depend on many factors.
My advice: If you're allowed to take the medicine, try it out.
If Buscopan PLUS is unable to alleviate your pain, then you have some alternatives: Ibuprofen/Diclofenac, Novalgin (Metamizol => prescription-only),
Spasuret* (Flavoxat),
Spasmex (Trospium chloride).
You'll find more information about painkillers for bladder inflammation under What painkillers help with bladder inflammation? and Which natural painkillers help with bladder inflammation?
Ibuprofen belongs to the group of non-steroidal anti-inflammatory drugs (NSAIDs). Ibuprofen blocks substances responsible for inflammation and pain. You can find out more about the anti-inflammatory ibuprofen under Does ibuprofen help with bladder infections?.
The maximum single dose for adults should not exceed 800 mg of ibuprofen. This corresponds to 400 mg IBU-ratiopharm, 2 film tablets. Prescription-only preparations are available up to 800mg per tablet, i.e. then accordingly max. 1 tablet per single dose.
Over a period of 24 hours, the Total dose should not exceed 1600 - 2400 mg of ibuprofen. The range of maximum doses is mainly determined by body weight. As an underweight person, you will tend to orient yourself more towards the maximum 1600 mg.
My experience: The agonizing pain of a bladder infection is hardly bearable! 1 tablet with 400mg does not help me at all I usually take 2 tablets of 400mg to begin with. In the daytime, I manage the pain better and try to reduce the dose or avoid taking medication altogether. Since I suffer most at night, I tend to take the maximum single dose of 2 tablets of 400mg before going to bed. Together with natural antibiotics such as Angocin® Anti-Infekt N* or D-Mannose*, I can sleep soundly.
Ibuprofen belongs to the largest group of over-the-counter painkillers, known as non-steroidal anti-inflammatory drugs (NSAIDs). Ibuprofen blocks substances responsible for inflammation, fever and pain.
An antibacterial effect of ibuprofen could only be shown in vitro studies. In one of these studies a clear antibacterial effect of ibuprofen was shown in the bacteria strains often responsible for bladder infections: Staphylococcus aureus, E. coli. It is still unclear whether this effect can be observed in humans in vitro.
Conclusion: Although ibuprofen may not show an antibacterial effect in humans, there are a few other reasons why the application (if possible) is not a bad approach:
Ibuprofen works
- pain-relieving
- inflammation-reducing
- just as effective as antibiotics for mild to moderate symptoms (according to a study)
The study "Immediate versus demand antibiotic therapy for uncomplicated urinary tract infection (ICUTI)" by the Institute of General Medicine at the University Medical Centre Göttingen and Hannover compared treatment with ibuprofen to antibiotic treatment with fosfomycin. Under ibuprofen, 70% of the included patients were symptom-free after one week (80% in antibiotic treatment).
More on the topic of painkillers for bladder infections can be found under Which painkillers help with bladder infections? and Which natural painkillers help with bladder infections?
A study compared a treatment with Ibuprofen to antibiotic treatment with Fosfomycin. Result: More than half were cured without antibiotics. However: In the study, women taking Ibuprofen had more symptoms and a higher risk of pyelonephritis.
My Conclusion: It is always unclear in advance whether you belong to the women who can be successfully treated or are complication-free without antibiotics. For me, this means that I use Ibuprofen as a pain reliever and anti-inflammatory. If no improvement is seen after about 3 days when combined with herbal remedies, I go to see my doctor and arrange for a urine culture. Ideally, I manage without antibiotics until the result of the urine culture (which can take a few days). If my symptoms do not improve by then, I can at least use the appropriate antibiotic that is sensitive according to the urine culture (and not just any old AB on a whim).
More information on pain relief for cystitis can be found under What pain relief helps with cystitis? and Which natural pain relief helps with cystitis?
The motto: As few medications as possible!
Pregnancy and breastfeeding are phases during which you should carefully consider taking painkillers (and medications in general), and you should always consult a doctor if in doubt.
The official information you will find in the package inserts:
- Paracetamol is safe throughout the entire pregnancy
- Ibuprofen only in the first and second trimesters (up to the 27th week of pregnancy)
- Acetylsalicylic acid (e.g. Aspirin®) only in the first 12 weeks of pregnancy
- Metamizole (e.g. Novalgin®) only in the first and second trimesters (up to the 27th week of pregnancy)
According to current knowledge, Ibuprofen is preferred in the first two trimesters for pain treatment in pregnant women. During breastfeeding, both Ibuprofen and Paracetamol are equally suitable.
In the third trimester of pregnancy, most painkillers, except for Paracetamol, are contraindicated. Under Ibuprofen, Metamizole, and other nonsteroidal anti-inflammatory drugs (NSAIDs), there may be fetal kidney damage as well as premature closure of the ductus arteriosus in the fetus in the third trimester.
For pain and high fever in the third trimester of pregnancy, Paracetamol is the treatment of choice. However, unlike Ibuprofen, it does not have anti-inflammatory effects.
What you need to know: As no randomized studies can be conducted on pregnant women, the available data on the effectiveness and safety of medications during pregnancy and breastfeeding are primarily based on experience.
During my research, I came across an interesting article from the Pain Clinic Kiel:
Paracetamol in pregnancy – Time to rethink.
The widespread belief: Paracetamol – You’re allowed! Take it! Take it, it won’t hurt! You can use it throughout the entire pregnancy. And it is believed that the correct dosage of the medication will cause no harm to mother or child. Paracetamol is very popular and
is a top-selling medicine.
The truth: Numerous studies have found a link between Paracetamol use in pregnancy and increased risks for the child for a whole range
of complications (e.g. severe developmental disorders, ADHD, HAS, cryptorchidism, asthma).
Poor benefit-risk ratio: It is now known that the therapeutic effectiveness of Paracetamol in pain treatment is negligible. With low effectiveness, one would think that the tolerability would be better. However, there are numerous risks as well: cardiovascular side effects, gastrointestinal ulcers, gastrointestinal bleeding, kidney dysfunction, elevated liver enzymes, twice the rate of liver transplant registrations, and severe skin reactions.
My conclusion: If you are pregnant, you should be aware that Paracetamol is largely ineffective for everyday pains (headaches, back pain). However, you still expose yourself to the risks if you take it!
Why take Paracetamol when it hardly relieves your pain but can put you and your child at risk?
In the German Pharmacists’ Newspaper (DAZ), you can find a tabular overview of possible painkillers during pregnancy and breastfeeding .
Here you will find an overview of possible painkillers for acute bladder infections or bladder irritation.
| Brand Names | Pain- relieving | Antispasmodic | Anti- inflammatory | Pregnancy | Breastfeeding | Prescription Required | Side Effects | |
|---|---|---|---|---|---|---|---|---|
| Ibuprofen | IBU-ratiopharm®Nurofen® | until 27th week of pregnancy | Stomach and bowel issuesAsthmaKidney damage | |||||
| Diclofenac | Voltaren® | until 27th week of pregnancy | Stomach and bowel issuesAsthmaKidney damage | |||||
| Metamizol | Novalgin® | weak | until 27th week of pregnancy | AgranulocytosisBlood pressure dropRash | ||||
| Paracetamol | Mexalen® | barely | Liver damageKidney damageAllergies | |||||
| Butylscopolamine | Buscopan® | AnticholinergicDry mouth | ||||||
| Flavoxat | Spasuret® | Not anticholinergicDigestive issuesDrowsinessDry mouth | ||||||
| Trospium Chloride | Spasmex®Spasmolyt® | AnticholinergicLiver damage |
General Note: This overview is not complete and does not replace the manufacturer information. Always check the package insert and consult with a doctor and/or pharmacist.
Note on Pregnancy (SS) and Breastfeeding:
no problems
application acceptable
short-term application/single doses acceptable
application not recommended or even contraindicated
Sources:
Test Strips
Most kidney and urinary tract diseases show a pathological change in the urine. A urine test strip is a very simple, non-invasive way to chemically analyze the urine, which can be self-performed outside of a laboratory (e.g. at home). With the urine test strip (synonyms: urinstix, urostix), a whole range of parameters can be determined. The determination and evaluation of the parameters is quick and simple by reading and comparing the test fields with the included control fields.
The most important pathological changes you want to detect are:
- Bacteriuria: high excretion of nitrite in the urine => clear indication of a urinary tract infection with nitrite-producing bacteria (e.g. E. coli, Klebsiella, Proteus Mirabilis)
- Leukocyturia: high excretion of leukocytes (more than 10 leukocytes/µL) in the urine => indication of an inflammatory disease of the kidneys or urinary tract
- Hematuria: high excretion of erythrocytes (blood) in the urine, which may not be visible in the urine (microhematuria) => considered a warning sign that should always be medically clarified.
- Proteinuria: high excretion of protein (albumin) in the urine => indication of kidney disease
- Glucosuria: high excretion of glucose (sugar) in the urine => indication of diabetes mellitus
Which fields indicate a bladder infection?
- Increased Leukocytes (usually shades of purple, the darker, the higher)
- Increased Nitrite (usually shades of pink, the more pink, the higher)
- Increased Erythrocytes (usually green dots or fully green)
- Increased Protein (usually shades of green): WARNING indication of kidney involvement!!
The following table describes the probability of a urinary tract infection:
| Test strip result | Urinary tract infection |
|---|---|
| Nitrite positive + Leukocytes positive | very likely |
| Nitrite positive + Leukocytes negative | very likely |
| Leukocytes positive + Blood positive | very likely |
| Nitrite negative + Leukocytes positive | likely |
| Nitrite negative + Leukocytes negative | less likely |
Other Test Fields (Parameters)
- Density (specific gravity): This provides a rough estimate of urine concentration. In cases of significant water loss, such as fever/diarrhoea/vomiting, the density is high. An increased density can also be a result of adrenal insufficiency, liver diseases, or heart failure.
-
pH value: Measure of the H+ ion concentration in the urine. High values can be caused by ammonia-producing bacteria in a urinary tract infection.
In general, the pH of urine is influenced by diet and medication.
- Normal range: 4.8-7.4
- Acidic urine: less than 7.0
- Alkaline urine: greater than 7.0
- Ketone bodies: Indicates that fat is being broken down in the body (e.g. during a diet). Ketoneuria can also occur in untreated diabetes.
- Urobilinogen: If elevated, it may indicate a possible liver disease, intestinal disease, anaemia, or heart failure.
- Bilirubin: Bilirubinuria (elevated levels) is a sign of jaundice, bile duct obstruction, or liver cell damage.
Other Procedures in Urine Diagnostics
Physical examination (volume, density, colour, smell, turbidity, foam), microscopic examination of urine sediment, urine bacteriology (determination of the type(s) of germs and germ count, determination of antibiotic sensitivity - antibiogram).
With the commercially available urine test strips (from a pharmacy or chemist), for example ELANEE Urine Control Test, Combur 5 Test Hc Test Strip or Combur 9 Test Test Strip, there is always an instruction leaflet provided. There it is described exactly what needs to be done next.
The steps in brief:
- Collect midstream urine
- Dip test stick briefly
- Wait 1-2 minutes
- Read the colour scale on the test fields
The steps in detail:
- Wash your hands and get a clean cup.
- Clean the intimate area (especially around the urethral opening)
- Midstream urine (preferably morning urine) in a cup while spreading your labia, collect.
- Dip the test stick briefly into the urine
- Wait 1-2 minutes for the colour change to stabilise
For a urine test using the rapid diagnostic technique, midstream urine is collected. What exactly does this mean?
By midstream we mean the middle part of the urine flow when emptying the bladder. We don't start collecting the urine from the beginning in a container, but rather after we've allowed some to run into the toilet first. Similarly, we don't collect the urine right up until the end of the voiding process, but withdraw the container before it's finished.
Important detail on the side: The urine stream should not be interrupted! i.e. simply hold the collection container in the urine stream after the first portion, don't 'stop' it beforehand!
Why do we only collect midstream urine? Because the first and last urine is often contaminated with bacteria from the urethral or vaginal opening. This can affect the reliability of laboratory results.
In normal circumstances, midstream urine is sufficient for everyday use. However, to ensure that the sample has no contaminants, doctors will often collect catheter urine (urine collected using a catheter) as well.
Keyword clean: Since we're particularly vulnerable to contamination, especially in the case of women, it's essential to have a clean sample. Therefore, before collecting your urine, follow these guidelines:
- Clean hands: Make sure you wash your hands thoroughly before handling the container and equipment.
- Clean container: Either use a sterile container or an individual, disposable cup.
- Clean urethral opening: With one hand, spread your labia and with the other hand, wipe the urethral opening from the clitoris to the vulval entrance using a clean, damp cloth.
- Clean sample: If you experience discharge or slime production during urination, insert a tampon before collecting your urine to ensure it's not contaminated.
Morning urine refers to the first urine produced in the morning. This urine is produced during the night and can be used as a specimen for testing. In contrast, spontaneous urine can be collected at any time of day or night.
Why would one want to use morning urine for a meaningful urine test? Morning urine is more concentrated and therefore better suited for bacterial tests, sediment analysis, and chemical analysis. Due to the longer dwell time in the bladder, it is also suitable for detecting nitrite (indicating a urinary tract infection) and proteinuria (indicating kidney disease).
Where is the problem in everyday life?
- The bladder inflammation does not always occur exactly before the first bowel movement in the morning.
- It is not advisable to store the morning urine for hours at home in a cup until visiting an outpatient clinic.
- When experiencing severe symptoms, one often drinks a little more and goes to the toilet frequently, including at night. As a result, the urine becomes less concentrated and less meaningful for testing.
My tips:
- In most cases, an acute, severe infection is strong enough for spontaneous urine to be sufficient for a diagnosis.
- To ensure the collected urine has spent as long as possible in the bladder, it's best to try to hold on for as long as possible before providing a specimen.
- If you have unclear symptoms (which may be more or less severe over time) or if a urine dipstick test does not react well and urine cultures are also not meaningful, I would definitely recommend using morning urine for testing. This will help you catch the culprits sooner.
Urine test strips are a genuinely simple and very quick method in urin diagnostics. However, one must say that the test can fail to be negative in up to a third of cases.
In plain language: In up to a third of women/men with urinary tract infections, the test will be negative and the urinary tract infection may therefore not be treated.
This inaccuracy has several reasons and few influenceable circumstances. For example, the urine may sometimes be too diluted to be meaningful. Example: If you have a urinary tract infection, drink a lot of water and feel like emptying your bladder every 10 minutes (and I can vouch for that from personal experience!), you will often not find nitrite to be present and the white blood cells will hardly be present.
The diagnosis becomes even more complicated when the bacteria are embedded and hide behind a biofilm. Then, the test strip will show nothing meaningful and even a urine culture may not find any bacteria.
My experience: When it "down there" suddenly starts to hurt and ache, then my gut feeling has rarely misled me. A urine test strip was often just the confirmation of what I had already suspected: a beginning urinary tract infection.
Where I find it helpful:
- Anti-hypochondriac: If you're starting to think your bladder is trying to trick you (which, given a condition like recurrent cystitis, is understandable), then a negative test can reassure you.
- The germ question: If nitrite shows up, it's likely mannose-sensitive bacteria.
- Follow-up control: If you're fighting an infection with non-synthetic antibiotics, you can see day by day whether you're on the path to recovery or if you should visit a doctor => with pyelonephritis, it's not to be taken lightly!
- Asymptomatic UTI: Do you hardly ever have symptoms when you have a urinary tract infection? Then test regularly with the test strips to get clarity.
Urine test strips are available from various manufacturers in different forms - available over the counter at pharmacies, chemists and online retailers. The more parameters (up to twelve substances per test strip) a urine test analyses, the more expensive the product is.
For at-home rapid diagnosis, in most cases the products with 5 parameters are sufficient, which are usually
- White blood cells
- Nitrite
- Protein
- Glucose
- Red blood cells
Well-known representatives are
- Combur 5 Test® Hc Test Strips*
- Combur® 9 Test Test Strips
- ELANEE® Urine Control Test
- Siemens Multistix
With the standard urine test strips available from pharmacies or chemists, such as ELANEE Urine Control Test or Combur 9 Test Test Strips, a packaging insert is always provided. It clearly describes what to do and how to interpret the results.
To make it easier to distinguish, each test field has its own characteristic colour. After soaking with urine and waiting for 60-120 seconds, the colour may have changed.
This changed colour is then compared with the control fields. The colour progression usually corresponds to the amount of chemical substance found.
In practice, the following colours have become established:
- Increased White Blood Cells (usually shades of violet, darker shades indicating higher levels)
- Increased Nitrite (usually shades of pink, pinker shades indicating higher levels)
- Increased Red Blood Cells (usually dots in green or fully green)
- Increased Protein (usually shades of green): WARNING Indicating kidney involvement!!
Urine test strips can measure up to 12 parameters at once. Not all values are relevant in terms of diseases affecting the urinary tract.
The parameters you should take a closer look at if you suspect a bladder infection:
- Increased white blood cells (usually shading in violet, the darker the higher) => indicative of an inflammatory disease affecting the kidneys or urinary tract
- Increased nitrite (usually shading in pink, the pinker the higher) => a clearer indication of a urinary tract infection with nitrite-forming bacteria (e.g. E. coli, Klebsiella, Proteus Mirabilis)
- Increased red blood cells (usually spots in green or fully green) => the presence of blood in urine is a warning signal that should always be clarified diagnostically.
- Increased protein (usually shading in green) => an indication of kidney disease (e.g. ascending bladder infection)
You can read more about what each parameter means here: What does the urine test strip say?
High Nitrite levels (=Bacterial Urine) and/or high Leucocytes levels (=Leucocytic Urine) suggest an acute urinary tract infection.
- High Leucocytes (usually shades of violet, the darker the shade the higher) => Suggests an inflammatory condition in the kidneys or urinary tract
- High Nitrite (usually shades of pink, the pinker the shade the higher) => A clear indication of a urinary tract infection caused by nitrite-producing bacteria (e.g. E. coli, Klebsiella, Proteus Mirabilis)
Nitrite positive + Leucocytes positive => Urinary tract infection highly likely
Nitrite positive + Leucocytes negative => Urinary tract infection highly likely
Nitrite negative + Leucocytes positive => Urinary tract infection possible (e.g. caused by Enterococcus)
Nitrite negative + Leucocytes negative => Urinary tract infection less likely
Some bacteria, like Klebsiella and Staphylococcus, do not produce nitrite. Therefore, a urinary tract infection caused by these bacteria may still show a negative nitrite result.
You can read more about what all the parameters mean here: What does the Urine Test Strip say?
Urine from a healthy person typically contains the following:
- no or up to 10 white blood cells/µL
- no nitrite
- no blood components
- only minimal protein traces (less than 0.15 g/l)
- only minimal glucose traces (less than 15 mg/dl)
The pH value usually ranges between 5-7 (strongly dependent on diet).
You can find out what all parameters mean in detail here: What does the urine test strip say?
You can read here what these values are: What positive test strip findings indicate a bladder inflammation?
Fresh, normal urine is clear and its colour can vary between light yellow to dark yellow (a mixture of yellow, reddish and brown pigments, known as "urochrome"). The colour also depends on the urine concentration.
Urine when suffering from a urinary tract infection
A change in colour can be caused by diseases (endogenous) or exogenous factors (e.g. medication, food). When you have kidney and urinary tract infections, the colour may turn reddish-brown due to blood presence.
Urinary tract infections can cause a cloudiness if large amounts of bacteria and white blood cells are present (pyuria).
Smell: When suffering from urinary tract infections, the urine may smell like ammonia (due to urease-producing bacteria) or have a foul odour (due to coliform bacteria).
Foam: If there is a persistent foam layer, it may indicate an increased excretion of proteins. This could be a sign that the kidneys are involved in a bladder infection.
General guidelines to avoid false results:
- Correctly stored test strips should be used.
- Clean cup without residues from disinfectants, clean hands, clean intimate area.
- Midstream urine from the morning urine (or at least 4 hours without urination before, otherwise it is too diluted).
- Fresh urine should be used for the rapid test (not older than 2 hours).
- Reading time should be strictly adhered to according to the package leaflet (usually after 1-2 minutes).
- Do not test during antibiotic or chemotherapy treatment (and not within 3 days after treatment with antibiotics or chemotherapy).
- Do not test during antibiotic treatment (and not within 3 days after antibiotic treatment).
- Erythrocytes are usually falsely positive during menstruation.
- Relatively large amounts of Vitamin C (ascorbic acid) can lead to false negative results.
Leukocytes
- False positive values can be caused by formaldehyde (disinfectant residue or after taking methenamine, e.g. Hiprex®).
- False positive values can occur from contamination with vaginal fluids.
- False positive values can occur from antibiotics (Imipenem, Meropenem, Clavulanic acid).
- False negative values can be caused by antibiotics (e.g. large daily doses of Cephalexin and Gentamicin (aminoglycosides), Nitrofurantoin, Tetracyclines (e.g. Doxycycline)).
- False negative values can occur from high protein excretion (> 5 g/L) (reaction color is weakened).
- False negative values can occur from high glucose excretion (> 20 g/L) (reaction color is weakened).
- False negative values can occur from high bilirubin excretion (reaction color is covered).
- False negative values can be caused by boric acid.
Erythrocytes
- False positive results are very common during menstruation (3 days before and 3 days after the period).
- False positive results can occur after intense exercise.
- False positive results can also occur from cleaning agents.
- Although the influence of ascorbic acid on glucose and blood has been largely eliminated in most test strips: False negative results can occur from large amounts of ascorbic acid (= Vitamin C).
- False negative results can occur from uric acid.
Nitrite
- Often unspecific false positive
- False positive results can occur from urine left standing for too long.
- False positive results can occur from dye in the urine (e.g. beetroot).
- False negative results can occur from medications containing phenazopyridine (pain reliever for alleviating symptoms in urinary tract irritation, brand names: Azo Standard, Pyridium, Prodium, Pyridiate, Baridium, Uricalm, Urodine, UTI Relief).
- False negative results can occur during antibiotic therapy (and up to 3 days after the last dose).
- False negative results if the urine is too diluted because it hasn't stayed in the bladder long enough (minimum 4-8 hours of urine retention in the bladder).
- False negative results can occur from a nitrite-poor diet.
- False negative results can occur from very acidic urine.
- False negative results can occur from non-nitrite-producing bacteria (e.g. Enterococci and Staphylococci).
- False negative results can occur from large amounts of ascorbic acid (= Vitamin C).
- False negative results can occur from high urobilinogen excretion.
Protein
- False positive results can occur after intense exercise.
- False positive results can occur during a general infection (e.g. cold).
- False positive results can occur with a urine pH > 9.
- False negative results can occur with a urine pH < 4.
pH value
- Alkaline urine (pH ≥ 7) can not only be caused by urease-producing bacteria but also by a vegetarian diet, overdose of baking soda*, disinfectant residues, or certain medications (e.g. Acetazolamide).
- Acidic urine (pH ≤ 5) also occurs in gout, acidosis, and fever.
False Results in Urine Culture for Bacteria
- Contaminated urine sample due to contaminated hands, contaminated cup, skin flora around the urethral opening, vaginal discharge.
- Urine sample not fresh enough and bacteria may have already proliferated by the time of testing.
- False negative result if the urine is too diluted because it was not in the bladder long enough (less than 4 hours).
- False negative result may occur with low-nitrite diet.
- False negative result may occur with non-nitrite-producing bacteria (e.g. Enterococci and Staphylococci).
| Leukocytes | Nitrite | |
|---|---|---|
| False Positive | Contamination with vaginal fluids Antibiotic: Imipenem Antibiotic: Meropenem Antibiotic: Clavulanic acid Formaldehyde after taking methenamine, e.g. Hiprex® | Urine left standing for too long Dye (e.g. beetroot) |
| False Negative | Antibiotic: Cephalosporins Antibiotic: Gentamicin Antibiotic: Nitrofurantoin Antibiotic: Tetracyclines Vitamin C High protein excretion > 5 g/L High glucose excretion > 20 g/L High bilirubin excretion Boric acid | Bladder retention time < 4h Strongly diluted urine Non-nitrite-producing bacteria, e.g. Enterococci e.g. Staphylococci Very acidic urine Vitamin C High urobilinogen excretion Low-nitrite diet |
There are two similar questions to this one that provide more accurate answers:
How reliable are urine test strips?
There are actually two similar questions that provide exact answers to this one:
How reliable are urine test strips?
The colour can be orange to reddish if there are blood mixtures present. (Note: If you have eaten red beetroot, this can also cause the urine to appear reddish.
Typically, the urine is muddy or cloudy.
In cases of kidney involvement, the urine may foam.
The smell can be reminiscent of ammonia or putrid.
You can find out what healthy urine looks like here: What does a healthy urine look like?
Bacteria in the urine can be identified by various methods, including culture and PCR (polymerase chain reaction).
Here are some of the most common methods used to identify bacteria in the urine:
Method 1: Urine Culture
In this method, a sample of urine is taken and placed on a special medium (agar plate) that allows the bacteria to grow.
The bacteria are then identified by their growth patterns and other characteristics.
Method 2: PCR (Polymerase Chain Reaction)
In this method, a sample of urine is taken and tested for specific genetic material (DNA or RNA) that is associated with the presence of bacteria.
The test can detect even small amounts of bacteria, but it cannot determine whether the bacteria are sensitive to antibiotics.
Method 3: Urine Culture and Sensitivity Testing
In this method, a sample of urine is taken and placed on a special medium that allows the bacteria to grow.
The bacteria are then identified by their growth patterns and other characteristics, and tested for sensitivity to various antibiotics.
It's worth noting that not all bacteria can be cultured or detected using these methods. In such cases, other tests may need to be performed to confirm the presence of bacteria in the urine.
Other Tests
Additional tests may also be performed to confirm the presence of bacteria in the urine, such as:
- Urine microscopy: This involves examining a sample of urine under a microscope for signs of bacteria or other microorganisms.
- Leukocyte esterase test: This is a quick and simple test that can detect the presence of white blood cells in the urine, which can indicate an infection.
A healthcare professional will advise on which tests are necessary to confirm the presence of bacteria in the urine.
Collecting a clean urine sample is not straightforward! As the urethra and the area around the urethral opening are colonised by bacteria, sample contamination with germs is often a problem. Additional criteria decide whether it's a case of contamination or an actual infection:
- Bacterial count: If more than 100,000 bacteria per ml are found, this is taken as a reliable indicator of a urinary tract infection.
- Symptoms: If the patient complains of symptoms, this is an indication of an infection, even if fewer than 100,000 bacteria/ml are present.
- Type of bacteria: If the urine culture finds more than two different types of bacteria or typical skin germs, then this points more towards contamination rather than an actual infection.
The symptom-free excretion of bacteria in the urine is known as asymptomatic bacteriuria. If different types of germs are found repeatedly in the urine or a urinary tract infection without symptoms is detected, then catheterised urine can be taken. This way, it can be ruled out that the sample has been contaminated with bacteria entering during urination.
False Negative Rapid Test
Considering that up to one third of all rapid tests give false results, it’s no surprise that according to the test strips in urine, nothing is often detectable (a false negative result). If symptoms persist, you can simply repeat the test to achieve a more accurate result.
The problem with the false negative urine test in the doctor's office: Your urine is usually not sent for a urine culture. This reduces your chances of identifying the pathogens.
Negative Urine Culture
There are often women who suffer from recurrent bladder infections/bladder issues, but no pathogen or no significant pathogen count is found in the culture. The reason could be that the bladder issues are actually not caused by bacteria. Or the pathogens might not be cultivable in a culture (e.g. gonococci and chlamydia). But more often, there’s another cause behind it: Embedded bacteria that hide in the bladder wall cells.
With a negative urine culture, you can alternatively try a PCR test (molecular biological examination) of the urine to detect the pathogens, such as the CystitisCheck at MVZ Institute for Microecology.
A more advanced version of the PCR test is the MicroGenDX Test, which combines the PCR test with Next-Generation DNA Sequencing (NGS) and can detect up to 50,000 pathogens.
Embedded Bacteria
The bacteria embedded in the cells are either just "sleeping" or they multiply like in a nest within the cell itself. Through the renewal of the bladder mucosa (urothelium), or the dissolution of superficial cells due to immune defense or simply due to mechanical irritation during sex, the nests are regularly uncovered. The bacteria then enter the bladder and repeatedly cause a bladder infection.
The bladder infection keeps coming back because the bacteria are released in bursts into the bladder.
Even antibiotics cannot affect the hidden bacteria (either in the urothelium or as a biofilm). The guideline-based treatment approach is long-term antibiotic therapy for at least 3 months, up to a year or longer.
Last Resort: London
I know many cases of recurrent bladder infections that are considered "treatment-resistant" in the DACH region, because no treatment attempt could resolve the bladder issue. Then it’s often concluded: Interstitial Cystitis (IC) or it is attributed to psychological problems. In fact, desperate patients ultimately even have their bladders removed because the constant pain is unbearable and the healthcare system offers no other option.
A private clinic at 10 Harley Street in London has been working on this issue for years with significant success. The summary of the treatment protocol: Long-term antibiotic therapy combined with methenamine (e.g. Hiprex®). Progress in the treatment is monitored via urine microscopy of fresh urine (= native sample, no urine sediment). This is measured by the number of leukocytes and epithelial cells found. You can find more information in the Facebook support group Embedded Bladder Infection Help and Exchange
Interstitial Cystitis (IC)
Constant pressure in the bladder, always urge to urinate, and a burning pain in the bladder area – and this day and night. With these symptoms, the diagnosis might be "Interstitial Cystitis" (the "rheumatism of the bladder") – a chronic, non-infectious bladder inflammation.
Explained in detail: In IC, the natural protective layer of the bladder wall is damaged. Irritating substances from the urine thus penetrate deeper tissue layers of the bladder wall, causing inflammation.
However, the diagnosis is a diagnosis of exclusion and can only be made once all other causes are excluded: bacterial infection, bladder stones, bladder cancer, endometriosis, overactive bladder. Even if the symptoms don’t occur at night, IC can be highly likely ruled out.
My Opinion: There is suspicion that an embedded bladder infection is often diagnosed as IC. Just because the bacteria are not found in a urine culture does not mean that the chronic inflammation is not caused by them. If the diagnosis of IC were in question for me, I would first seek treatment in London before undergoing the sometimes painful diagnostic and treatment attempts for suspected IC.
During treatment with antibiotics and up to three days afterwards, the urine test is not meaningful. In particular, the fields for white blood cells and nitrite may show false results.
White blood cells:
- False positive: Antibiotics containing the active ingredients imipenem, meropenem and clavulanate.
- False negative: high daily doses of cephalosporin antibiotics (e.g. cephalexin), gentamicin (aminoglycosides), tetracycline (e.g. doxycycline), nitrofurantoin
Nitrite:
- False negative: The formation of nitrite may be disturbed after taking antibiotics.
Due to the lack of detection of lymphocytes during antibiotic intake, it is recommended to determine the white blood cells in the urine sediment.
Protein: Protein in the urine may occur as a side effect during antibiotic treatment. Even with the use of painkillers from the NSAID group (non-steroidal anti-inflammatory drugs such as ibuprofen), the protein value in the urine can be increased.
As filter organs, the kidneys are responsible for producing urine. If there is an increased amount of protein in the urine (=proteinuria), it usually indicates kidney diseases or kidney damage. Additional symptoms of illness can include a frothy appearance, increased yellowing of the urine or fluid accumulation in tissues.
Bladder infection: Apart from this, there are several other causes for protein in the urine, including bladder infections and urinary tract infections. In these cases, the albumin (smallest protein particle) in the urine may be temporarily increased. With a bladder infection, there is an increase in bacteria and inflammatory cells in the urine. Since both the bacteria and the inflammatory cells are largely made up of proteins, this often leads to an increased excretion of protein.
Other diseases that can lead to proteinuria include autoimmune diseases, diabetes mellitus and other metabolic disorders, heart failure, high blood pressure, infections, side effects of medications (antibiotics and painkillers in the NSAID group).
The protein excretion can also be increased by partially harmless causes such as: low fluid intake (dehydration), stress, physical exertion, fever or hypothermia, pregnancy, menstrual bleeding. Pains
Zero to ten white blood cells per microlitre are considered negative. In other words, if you have more than ten white blood cells per microlitre in your urine, the test is positive (leucocyturia).
You can read about what these parameters mean: What does a urine dipstick test reveal?
Here you can see how reliable the parameters are: What can skew the results of a urine dipstick test?
A positive test strip finding for nitrite is likely to indicate a urinary tract infection. Nitrite is produced as a breakdown product of bacteria in the urine.
You can read more about what these parameters mean here: What does my test strip say?
You can also learn how reliable the parameters are here: What can affect the accuracy of my test results?
With significantly elevated leukocyte levels in the urine (leukocyturia => more than 10 white blood cells per microliter) without the detection of bacteria, there can be many reasons:
- False positive rapid test: Here you can read about how reliable the parameters are => What can distort the urine test?
- Urethritis (inflammation of the urethra): Inflammation of the mucous membrane of the urethra caused by (very often sexually transmitted) bacteria such as gonococci, chlamydia, mycoplasmas, ureaplasmas, trichomonads (single-celled organisms). Intestinal bacteria can also cause urethritis. A sign of urethritis is a higher leukocyte count in the first 10 to 15 ml of urine (=> two-glass test)
- Fungal infection: Mostly Candida species, but also Aspergillus => Detection by microscopic urine examination.
- Parasitic infection: Urogenital schistosomiasis (bilharzia) => Microscopic detection of schistosomes
- Infection with rare pathogens: Non-tuberculous mycobacteria, anaerobes (Peptococcus and Peptostreptococcus), Gardnerella vaginalis
- Viral infection: The herpes simplex virus can infect the urethra, cause pain during urination, and cause problems when emptying the bladder. . A BK-(polyoma) virus infection can lead to a bladder infection with heavy, visible blood in the urine in immunocompromised patients.
- Biofilm: Bacterial colonies protected by a self-generated extracellular polymeric matrix, the biofilm.
- Embedded bacteria: Intracellular bacterial communities => Uropathogenic bacteria can also penetrate the urothelial cell and form a biofilm-like community there. This protects the bacteria from the immune system, triggers recurrent urinary tract infections, and can cause symptoms even if standard diagnostics do not detect a urinary tract infection. More on this topic at Is a bladder infection always detectable in the urine?
Certain germs require a special culture medium (culturing bacteria on special culture media) or a special detection method
(e.g. microscopic pathogen detection, polymerase chain reaction [PCR], detection of bacterial antigens, indirect detection via specific antibodies in the blood) to be detectable.
These include:
- Anaerobes
- Gardnerella vaginalis
- Neisseria gonorrhoeae (gonococci)
- Chlamydia tranchomatis (chlamydia)
- Mycoplasma huminis (mycoplasma)
- Ureaplasma urealyticum (ureaplasma)
- Herpes simplex (virus)
- Candida (fungi)
- Trichomonas vaginalis (trichomonads)
- Schistosoma haematobium (urogenital bilharzia)
Special tests should always be requested when a urinary tract infection is highly likely but the urine culture has not revealed the pathogen.
Nitrite negative, but leukocytes positive suggests that a urinary tract infection is likely. Nitrite is very unstable and certain bacteria do not produce nitrite (Enterococci, Staphylococci). Leukocytes always indicate an inflammation.
You can read here what the parameters mean: What does the urine test strip say?
You can read here how reliable the parameters are: What distorts the urine test?
A positive result is always an indication of a bacterial urinary tract infection. However, a negative result does not mean that there are no bacteria in the urine.
Why the nitrite field is prone to interference:
- Bacteria count: There are too few bacteria in the urine and the field does not react. Or there are an excessive number of bacteria in the urine and the nitrite is broken down by the bacteria themselves.
- Type of bacteria: Not all types of bacteria can produce nitrites, such as Staphylococcus, Enterococcus, Pseudomonas, Gonococcus, or Mycobacteria.
- Large urine volumes: If the urine is very diluted due to large fluid intake. Therefore, it's best to test concentrated morning urine.
- Residence time in the bladder: Nitrite production requires time. The result is not reliable if the urine has not remained in the bladder for at least 4 hours.
- Antibiotics: During antibiotic treatment, nitrite production can be disrupted.
- Lack of nitrates: If there is a lack of nitrates in the urine (one-sided diet without vegetables, malnutrition), the bacteria do not have the raw material to produce nitrites.
You can read here what the parameters mean: What does a urine test strip say?
You can read here how reliable the parameters are: What falsifies the urine test?
Here you can read why nitrite often doesn't trigger: Why does the nitrite stay negative despite urinary tract infection often?
The increased excretion of red blood cells (=erythrocytes) is referred to as haematuria. This occurs at a concentration of > 5 erythrocytes/µL. Lysed erythrocytes (=haemoglobin) colour the test field evenly (uniformly) green. Intact erythrocytes result in green, pinpoint colour reactions.
If the positive result is not due to menstrual bleeding, or for example after intense exercise, blood in urine always indicates a warning sign and has a pathological cause in the urogenital tract in most cases.
Possible causes of blood in urine:
- Inflammations: e.g. glomerulonephritis (kidney inflammation), pyelonephritis (kidney pelvis inflammation), cystitis (bladder inflammation).
- Stones: kidney stones, ureter stones, bladder stones.
- Tumours & Cysts: kidney tumour, ureter tumour, bladder tumour, prostate tumour in men, cystic kidney, renal cysts.
- Injuries: injuries to the kidneys and urinary tract (including catheterisation and bladder examination).
- Antibiotic use: during antibiotic therapy, nitrite formation can be disrupted.
- Prostate adenoma: benign enlargement of the prostate in men.
Good to know: Due to mechanical irritation during sex, blood in urine can be found in up to a quarter of women the next morning.
You can read more about what protein in urine might mean here: Does having protein in your urine indicate a bladder infection?
Here, you can learn about all the parameters and what they mean: What does my urine test strip say?
Here, you can find out how reliable the parameters are: What can affect the accuracy of the urine test?
A glucose level of over 15 mg/dl in the urine is referred to as glucosuria. Diabetes mellitus is the main and most common cause of this condition. When blood sugar levels reach around 160 mg/dl, sugar can be detected in the urine. Kidney diseases can also be a cause of elevated glucose in the urine.
Pregnancy: Even with relatively low blood sugar levels, glucose is excreted in the urine (kidney threshold for glucose drops during pregnancy). However, a positive result must still be clarified to determine if you have gestational diabetes and take action accordingly.
You can read more about what all the parameters mean here: What does the urine test strip say?
You can also read how reliable these parameters are here: What can distort the urine test?
The following products are from well-known manufacturers: Combur® 9 Test Test Strips, ELANEE® Urin-Kontrolltest, Siemens Multistix®.
There are now also cheaper urine test strips from many other manufacturers, for example: One+Step Urin Test Strips*.
More information can be found under: What test strips should I use with bladder inflammation?
As a rough guide: Nitrite-producing bacteria are mannose-sensitive (except Proteus Mirabilis). This means that if your nitrite field is negative (no colour change), then D-mannose will probably have no effect.
But: Nitrite is a very unreliable parameter. It is often falsely negative. I would still try to take D-mannose until a urine culture has accurately identified the bacteria / microbes in your system. D-mannose* has virtually no side effects and is not too expensive in its simple, pure powder form.
More on D-mannose* at: When does D-mannose help? / Which bacteria does D-mannose help?
You can read here how reliable the parameters are: What falsifies urine testing?
Generally speaking: The fresher, the better.
Urine for dipstick testing should be used as fresh as possible, and certainly within a 2-hour time frame. Before submission to the laboratory or practice, the urine should be stored in a cool place (i.e. at 2-8°C in a refrigerator).
If left for longer periods, many of the values will be falsified and make the sample unusable. Even for urinalysis, the urine should be as fresh as possible since bacteria in the urine can multiply rapidly at room temperature and lead to false-positive results.
No!
So my advice is: Test strips at the time of reading (usually after 60-120 seconds, see package insert) take a photo with your phone to photograph, so you can then analyse in peace, by comparing the photo with the comparison scale on the packaging.
More information can be found under Is cystitis always detectable in urine?
If the test strip is clean and no other symptoms or complaints occur, it is most likely a contaminated sample, which usually occurs due to an incorrect specimen collection. So, if there are flecks in your urine without any complaints, it's usually unnecessary to worry.
- Cleansing: Did you clean the area around the urethral opening before taking the sample?
- Vagina: Were your labia separated during the sampling process?
- Middle stream urine: Did you actually collect mid-stream urine?
If the sample was taken correctly, white flecks/flakes can also have the following causes:
Tip: If a urine sample appears to be contaminated repeatedly, you may want to consider having your doctor analyse catheterised urine in doubt.
The pH level of urine indicates the acidity, more precisely, the concentration of hydrogen ions (H+). In healthy individuals, it typically ranges between 4.8 and 7.6.
The pH of urine provides a rough indication of the acid-base balance of the body and can also indicate urinary tract infections.
- < 6.5 => acidic (acidotic) urine
- > 6.5 => alkaline (basic) urine
What can be deduced from a high pH level?
- Possible urinary tract infection: Some bacteria can produce ammonia (nitrite-producing (=urease-producing) bacteria). Ammonia alkalizes the urine.
- Alkalosis of the body: e.g. due to hyperventilation, vomiting, potassium deficiency, overuse of antacid medications
- With a vegetarian diet, the pH level can be higher
What can be deduced from a low pH level?
- Acidosis (over-acidification) of the body: e.g. due to reduced exhalation of carbon dioxide from lung disease, diarrhea, poisoning, starvation, diabetes, kidney damage
- With a high-protein (meat-rich) diet, the pH level can be lower
Reasons for acidification: When would you want a low pH level?
- For prevention after a healed bladder infection (as studies on this show conflicting results, it is not recommended in the current S3 medical guidelines)
- In acute UTI with Staphylococcus, Enterococcus, Streptococcus
- During antibiotic treatment with Fosfomycin, Nitrofurantoin, Penicillin, Sulfonamide (e.g. Cotrim)
Reasons for alkalinization: When would you want a high pH level?
- In acute UTI with E. coli, Proteus mirabilis, Klebsiella, Pseudomonas aeruginosa
- For pain relief in an acute UTI (reduces the burning sensation during urination)
Since the acidity (pH level) strongly depends on diet, you should first know your personal "normal state". This can be done using pH test strips (e.g. inexpensive litmus paper strips), which allow you to measure your pH level several times a day for several days (in a healthy state, not during a UTI or antibiotic treatment).
It is completely normal for the pH level to fluctuate during the day (a "rise and fall"). In the first morning urine, it is usually in the slightly acidic range (around 6.3 to 6.5), and after a meal, it is typically temporarily increased (1 to 2 hours after meals, at least 6.8).
The pH of the urine is usually between 4.8 and 7.6.
- < 6.5 => acidic (azidotrophic) urine
- > 6.5 => alkaline (alkalotic) urine
To measure the acidity level, you collect midstream urine and then hold a test strip into it. Alternatively, you can hold the test strip directly in the urine stream.
There are two types of pH testing strips available:
- Indicator sticks with reaction areas, such as pH-FIX indicator sticks.
- Value for money: Lackmus indicator paper without reaction fields (the paper changes colour), such as Uralyt-U indicator paper.
My tip: You can easily double the number of strips in a pack by cutting each strip in half. Half a strip is sufficient for the test.
To make a statement about the acid-base balance, a daily record must be kept for one week.
In a so-called "urine pH profile of the day", multiple measurements are taken throughout the day, starting with the first morning urine, further measurements every 2-3 hours until bedtime. After meals, at least 2 hours should be waited before taking the next measurement. After a week, the protocol can be evaluated.
A alkalisation of the body is assumed if the
- pH value of the first morning urine always lies below 6.0
- the average pH value of the day's profile lies below 6.3 (Average of all measurements of a day's profile)
The pH level of urine fluctuates throughout the day, with a constant "up and down".
A high pH level indicates alkaline urine (pH level > 6.5). This could be due to:
- Possible urinary tract infection: Certain bacteria produce ammonia, which alkalises the urine.
- Body alkalosis: e.g. hyperventilation, vomiting, potassium deficiency, or taking too many stomach acid neutralisers
- 1-2 hours after a meal
- A vegetarian diet
Urine with a pH value of 7 is clearly alkaline. You can read about when the urine is alkaline here: What happens if the pH value in urine is increased?
In medical training, it has been taught for a long time that acidifying the urine can suppress recurring bladder infections. A well-known preparation for acidification is the essential amino acid L-Methionine (e.g. Acimethin®, Acimol®).
L-Methionine should, on the one hand, inhibit the growth of uropathogenic bacteria. On the other hand, it should also be able to reduce the ability of the bacteria to adhere to epithelial cells in the urinary tract and make it more difficult for them to penetrate the cell. The best effect is expected at a urine pH between 5.8 and 6.2.
Since this theory is not sufficiently supported by studies, acidifying the urine is not recommended as a measure in the medical guidelines.
But what about natural remedies? One alternative to the already mentioned products with L-Methionine is high-dose vitamin C (ascorbic acid).
Dosage: Take 3-4 times a day, 2-3 g of vitamin C. It's essential to note that it must be ascorbic acid and not, for example, vitamin C from the Acerola cherry, as this does not acidify.
To ensure that the acidification is effective, you can easily control the pH value of your urine multiple times a day using test strips. More information on this can be found under How can I measure the pH value of my urine?
In the article Erregerkompass, you will find more information on which natural remedies help against different bacteria.
There are many fellow sufferers who alkalise their urine (e.g. with Natron*), so that the burning sensation in the bladder during an acute urinary tract infection is milded. This usually works, but is counterproductive if the infection is caused by a different type of bacteria.
So how do you make your urine alkalise? Take baking soda/Natron* or lemon/lime juice with water.
Dosage: With each glass of water (250ml) take 2 tablespoons of lemon juice
and a teaspoon of baking soda (sodium bicarbonate).
To make sure the alkalisation works, you can easily control the pH level of your urine several times a day with test strips, more information about this under How can I measure the pH level of my urine?
In the article Infection compass you will find more information about which natural remedies are most effective against different types of bacteria.
You can find more information about this under When should I make / alkalisise my urine?.
Find out more about this under When should I make my urine acidic?.
You can find some general information about this under When should I make my urine alkaline / alkalisify?.
Just because something tastes sour, it doesn't mean it will be acidic in the body. The same applies to alkaline foods. The acidity of a food does not determine whether it is acidic or alkaline when metabolized by the body - its pH value in the body is always the result of metabolic processes.
Most citrus fruits are sour, but they have an alkalising effect on the body. Chocolate cake itself is alkaline, but produces acid in the body.
The following foods will have an alkalising effect on the body:
- Most fruits (with lemons leading the way)
- Green vegetables
- Lentils
- Herbs and spices
- Seeds
- Baking powder/ Natron*
- Mineral water
You can find detailed tables on the alkalising and acidifying effects of various foods on this website:
Some general information can be found on When should I make the urine alkaline / alkaliise it?.
Just because something tastes sour, it doesn't mean that it will have a sour effect in the body. The same applies to alkaline foods. The acid content of a food does not determine whether it is acidic or alkaline in the body => its pH value in the body is always a product of metabolic processes.
Most citrus fruits are sour, but have an alkaline effect on the body. Even chocolate cake itself is alkaline, but produces strong acidity in the body.
The following foods produce acidity in the body:
- Meat
- Fish
- Poultry
- Eggs
- Grains
- Legumes
- Alcohol
- Coffee
- Artificial sweeteners
You can find detailed tables on alkaline and acidic foods on this website.
You can find more information about this under When should I make / alkalisise the urine?.
All the information is available under When should I acidify my urine?.
pH test strips come in two forms:
- Indicator sticks with reaction fields, e.g. pH-FIX indicator sticks
- Cheap: litmus paper without reaction field (the paper changes colour), e.g. Uralyt®-U litmus paper
My tip: Cheap litmus paper does the job and is relatively very cheap (about 1p per strip).
More information under How can I measure the pH value of urine?
In a healthy vaginal flora, the acidic environment (pH level between 3.8 and 4.4) created by lactobacilli ensures that harmful bacteria cannot survive. This acidic environment is not only a protective barrier against vaginal infections but also protects against bladder infections. If the vaginal pH balance is disrupted, it becomes easier for bacteria to enter the urethra and trigger a bladder infection.
Conclusion: Do you suffer from recurring urinary tract infections or vaginal infections? It's worth keeping an eye on your vaginal pH level then. And you can do that with vaginal pH test strips (pH test strips integrated into vaginal applicators), e.g. ELANEE® pH Test. If the pH value is 4.5 and higher, you should take action urgently. Here you'll find tips on how to restore your vaginal flora to a healthy state: Vaginal Flora, Intimate Hygiene, Gynaecologist/ Gynaecologist.
If none of the tips and tricks help to get your vaginal environment back into balance, please consult a doctor. There, an antibiotic therapy with e.g. Clindamycin or Metronidazole can be initiated (as cream, vaginal suppositories or tablets as well as tablets to take).
Vaginal pH levels in the range of 3.8 to 4.4 are within the normal/healthy range.
Temporary increases can occur during menstruation and after sex (menstrual blood and semen have a pH level of more than 7, which is basic). Normally, your body will correct these fluctuations on its own.
If your vaginal pH level, however, remains outside the normal range for a longer period and you are experiencing additional symptoms (itching, fluid discharge with a fishy odour, recurring bladder infections), it is time to establish a healthy balance of bacteria in your vagina or visit your gynaecologist for treatment with antibiotics.
You can read more about this here: Vaginal flora, Intimate hygiene, Gynaecologist.
A healthy vagina is acidic and rich in lactic acid bacteria (=lactobacilli). The pH value of a healthy vagina lies between 3.8 and 4.4. This acidic environment offers poor living conditions for foreign organisms and is also a natural barrier against vaginal infections and bladder inflammation. The natural vaginal flora thus has an important function in defending against pathogenic bacteria and fungi.
If the acidic pH value of the vaginal flora becomes unbalanced (such as through excessive intimate hygiene, stress, oestrogen deficiency, antibiotics), the beneficial lactobacilli in their development are hindered and pathogenic organisms can multiply much more easily. These pathogens can then easily enter the urethra and trigger a bladder inflammation.
A lack of protective lactobacilli disturbs the balance of vaginal flora and leads to a pH value shift in the vagina from the healthy, acidic range (between 3.8 and 4.4) to the alkaline range at 5.0 or higher.
In the more alkaline environment, numerous (even physiologically living) microorganisms now find ideal conditions for growth, or from outside (near the anal area, sexual intercourse) to invade. A so-called vaginal bacteriosis (disruption of the natural vaginal flora balance) can also be caused by a mixture of various microorganisms . Most often, the bacterium Gardnerella vaginalis is involved.
An imbalance in vaginal flora also always brings with it the risk of urinary tract infection. That's why it's so important for all women with recurring bladder infections to have a healthy vaginal environment.
Here you'll find tips on how to bring your vaginal flora back in balance: Vaginal flora, Intimate hygiene, Gynaecologist.
Do you suffer from recurring urinary tract infections and/or vaginal infections? It's worth keeping an eye on your vagina's pH value then. And you can do that with vaginal pH test strips (integrated pH test strips in vaginal applicators), e.g. ELANEE® pH Test.
The applicator is inserted into the vagina like a tampon and pressed against the back wall of the vagina for about 10 seconds in the direction of the intestines, not towards the bladder. This ensures that the measurement area is well moistened to determine the pH value. The result is read immediately after removing the applicator from the vagina by comparing the colour of the pH measurement area with the colour scale on the packaging/leaflet. The pH value indicated by the colour closest to your measurement area is the result.
If the pH value is below 4.5 and you still have symptoms of an infection (itching, burning, unusual white or scabby discharge), it may be a fungal infection.
If the pH value is 4.5 or higher, it could be due to a bacterial vaginosis or imbalance, and you should take action urgently. Here's how you can get your vaginal flora back on track: Vaginal flora, Intimate hygiene, Gynaecologist.
Vaginal pH test strips are available in pharmacies, health food stores and online. A well-known representative is ELANEE® pH-Test.
I am currently using ellen® pH-Control® and I am satisfied with it.
My tip: Vaginal pH test strips are not really cost-effective (depending on the packaging size, up to more than £4 per test) Cheap litmus paper indicator paper serves just as well if you use a sterile glove (or clean fingers) to take fluid from the vagina and apply it to the test strip.
Antibiotics
Suitable antibiotics help well, but are not always necessary.
In the case of an uncomplicated bladder inflammation, the spontaneous healing rate is reportedly around 30-50% after a week according to studies (after one week, 30-50% of all acute, uncomplicated HWI's heal by themselves without antibiotic treatment). This means that at least one-third of all acute, uncomplicated UTIs will resolve on their own without antibiotic treatment.
As a result, the main focus in treating an uncomplicated bladder inflammation is to get the clinical symptoms under control more quickly (e.g. with plant-based medications and pain relief medication like ibuprofen).
When does one speak of an uncomplicated bladder inflammation? The majority of uncomplicated cases are those in which the infection has not spread to other parts of the urinary tract.
Conclusion: A UTI is suitable for self-medication only in uncomplicated cases.
My experience: Online, one often finds that it can take several weeks for a bladder inflammation to heal on its own. If my symptoms and the urine test strip have not improved after 3-5 days of self-medication without AB (antibiotics) have not changed noticeably, I have always ended up taking antibiotics.
My tip in case of first signs of a UTI: Go to the doctor and get your urine tested, and have it sent for culture and sensitivity testing. If you still try to tackle the problem with natural remedies after a few days, that's fine! But if not, then at least you will have an antibiotic treatment plan with the list of susceptible antibiotics for your bacteria (your germs) ready.
Until just a few years ago, antibiotics were the standard therapy for bladder infections, even for uncomplicated ones. I can confirm this from personal experience.
However, it is now known that the uncritical use of antibiotics is a serious mistake – even though the quick relief of symptoms through antibiotic use is very tempting.
Warning: Resistance Development: When antibiotics are taken indiscriminately and are also used extensively in livestock farming, resistance development increases. Infections with (multi)resistant bacteria are often severe and sometimes even incurable. In the EU, more than 30,000 people die each year from such infections.
Warning: Microbiome: Another reason to question the repeated use of antibiotics is the gut microbiome. Bacteria are not inherently harmful but are, in fact, a necessary component of a healthy organism. The prolonged use of antibiotics can severely impact the gut flora and lead to health problems elsewhere in the body.
Warning: Side Effects: Antibiotics generally have more side effects than phytopharmaceuticals. These range from typical gastrointestinal issues to permanent side effects such as nerve damage with fluoroquinolones (Ciprofloxacin, Norfloxacin, etc.).
The Underestimated Danger - Embedded Bladder Infection:
From my experience working with various advisory groups, I know of many women whose bladder infections keep recurring despite all possible attempts at treatment,
or whose bladder remains permanently inflamed, even when a urine culture cannot detect any bacteria.
The bladder infection has, in a sense, become chronic.
The likely cause: The bacteria hide in the deeper layers of the bladder lining and in biofilms, where they are
resistant to antibiotics.
And how does this happen? The longer the germs remain untreated or unsuccessfully treated in the bladder,
the better they can establish themselves and eventually embed.
The resulting vicious cycle: With the renewal of the bladder lining, the "dormant" bacteria return to the bladder,
triggering an infection again, where they multiply
unchecked without treatment. Some of the new bacterial load re-embed in the lining. The cycle begins again.
Why am I telling you this? Because a targeted treatment with the appropriate antibiotic
(i.e., exactly what is sensitive to your specific bacteria, as indicated by a urine culture & antibiotic susceptibility test)
before they can embed and then torment you with painful infections for months or even years.
isn't a bad idea and ensures that the uropathogenic bacteria are "nipped in the bud"
before they become entrenched.
Such cases are often quickly considered "untreatable" in DACH, and some desperate women even agree to have their bladder removed.
A urological private clinic in London (Professor Malone-Lee †)
fortunately has a treatment plan for such cases.
More on embedded bladder infections and the London treatment protocol
under Is a bladder infection always detectable in urine?
Here is an overview of the pros and cons:
| Herbal Therapy (+ Painkillers) | Antibiotic |
|---|---|
| slow symptom relief | faster symptom relief |
| slightly increased risk of kidney infection | rare kidney infection |
| chronicisation (embedding) possible | chronicisation (embedding) rare |
| no damage to the microbiome | possible damage to the microbiome |
| few side effects | sometimes severe side effects |
| no resistance formation | possible resistance formation |
To start off with the topic of antibiotics, I recommend reading this in advance:
What are the pros and cons of antibiotic treatment?
Given the facts that up to two-thirds of uncomplicated urinary tract infections can heal spontaneously without antibiotics and the global development of resistance to antibiotics by bacteria can become a fundamental problem, it is recommended to try non-antibiotic treatments first for an uncomplicated urinary tract infection.
BUT - There is a kind of checklist that will make the decision "Antibiotic - Yes or No?" easier for you. The more of the following questions you can answer with YES, the more important it may be for you to use antibiotics:
- Are you in a risk group (child, man, pregnant woman)?
- Are you in menopause?
- Do you suffer from recurrent urinary tract infections (more than 3 UTIs per year or more than 2 UTIs in half a year)?
- Do you have comorbidities such as functional or anatomical urinary tract disorders, diabetes, kidney dysfunction, or immune deficiency?
- Do you have symptoms suggesting kidney involvement? For example, flank pain, painful kidney area, fever >38°C, chills, nausea, or vomiting.
- Have your symptoms not improved after 3-5 days?
- Do the test strips on a urine test strip show elevated values for leukocytes and/or nitrite and/or blood?
- Is a bladder or urinary tract examination planned (this is generally not done during an acute infection)?
Participatory decision-making: The best treatment option should always be discussed and decided together with your doctor.
My tip - or rather - my command 🙂 to you:
On the internet, you often find that it can take several weeks for a urinary tract infection to heal on its own. If my symptoms and the urine test strip during self-treatment without antibiotics have not noticeably improved after 3-5 days, I have found that antibiotics have ultimately been necessary - even though I "fiddled around" for several weeks.
The command is therefore - and yes, I also have to pull myself together: 🙄
If you suspect a urinary tract infection, go to the practice, have your urine (preferably morning urine) tested and insist that the urine sample is sent for a urine culture with antibiogram
to a laboratory.
Are your symptoms severe and you don't know if you can hold on until the culture results?
Then ask your doctor to give you an emergency antibiotic (this falls under "calculated therapy" - it’s an antibiotic that, for example, has worked for you before in a UTI, or generally
has a broad spectrum of action and is recommended for UTIs according to guidelines). Only take the emergency antibiotic if you truly cannot wait for the antibiotic results from the antibiogram.
(Note: The antibiogram usually takes 2 - 4 days because the bacteria must be cultured on a growth medium and then tested for resistance against a range of antibiotics per grown bacterium).
Ideally, you would take an antibiotic according to the antibiogram that is sensitive to your bacteria even for an uncomplicated urinary tract infection, if necessary. If there are several options, choose the one that is best tolerated (no contraindications such as allergies, comorbidities, etc.) and has the fewest side effects & collateral damage (An example: the broader the spectrum, the more types of bacteria are destroyed, even where you need the bacteria, such as in the gut).
A summary table of recommended antibiotics for uncomplicated cystitis (including assessment of side effects, collateral damage, etc.) can be found here: S3 Guideline: Uncomplicated Urinary Tract Infections
You are probably asking yourself - Why should I go to all this trouble?
If you recover in a few days with natural remedies, wonderful!
You don't need to take any antibiotics.
But if the infection does not improve or even gets worse, at least you will have an antibiotic available that is sensitive to your bacteria
- even on weekends or public holidays.
In case of emergency, this process will save you a lot of suffering and protect you from a chronic urinary tract infection.
There are a number of antibiotics used for urinary tract infections. The medical S3 guidelines also provide clear recommendations on this.
Bladder infections (and subsequently kidney infections) are caused by various pathogens. Therefore, first and foremost: Not every antibiotic works for every pathogen. This is also why you should always urge your treating doctor to carry out a urine culture + antibiogram to determine the pathogen and the effective antibiotics when you present with symptoms of a bladder infection.
You might be wondering: If knowing the pathogen is so essential for treatment, why on earth doesn’t the medical staff encourage this right from the start? => Because the guidelines do not recommend it and because it is costly. Instead, a so-called "calculated therapy" with a "best guess antibiotic" is initiated.
The "best guess antibiotic" is usually chosen based on these criteria:
- Risk: Which patient group do you belong to? Are you pregnant? Do you already have symptoms of kidney involvement?
- Sensitivity: Which antibiotics are already resistant in your region?
- Pathogen spectrum: Against which (suspected) pathogens should the antibiotic work?
- Effectiveness: What percentage of pathogens are destroyed by a standard dose of the substance?
- Side effects: What unwanted side effects might occur due to your medical history (known allergies, kidney dysfunction, liver disease, etc.)
- Resistance situation: Is there a risk of collateral damage (resistances in you or the population)?
- Antibiotic Stewardship: Rational and responsible use of antibiotics => no reserve antibiotic should be used for an uncomplicated infection
By adhering to the above criteria, the following antibiotic groups should not be used for a purely "calculated therapy":
- Fluoroquinolones (all antibiotics ending in -floxacin): Serious side effects possible, collateral damage through the formation of multi-resistant pathogens
- Cephalosporins (all antibiotics starting with Cef-/Ceph-): Collateral damage through the formation of multi-resistant pathogens
- Fosfomycin (e.g. Monuril®): Intravenous use is considered a reserve antibiotic , therefore oral intake is not the first choice (even though it is an effective antibiotic and the guidelines classify it as preferred)
- Trimethoprim (e.g. InfectoTrimet®), Trimethoprim + Sulfamethoxazole (Cotrimoxazole): If the regional resistance situation for Escherichia coli is > 20 percent
So what remains, if the pathogen is unknown and you’re looking for an antibiotic to treat uncomplicated cystitis that works as effectively as possible - with few side effects and minimal collateral damage?
- Nitrofurantoin: Furadantin®, Nifuretten®, Nifurantin®, Uro-Tablinen® => very broad spectrum with exceptions: Proteus mirabilis and Pseudomonas aeruginosa are naturally resistant to Nitro (!)
- Nitroxoline: Nitroxoline forte, Nilox®
- Pivmecillinam: X-Systo® (Germany), Selexid® (Austria) => may also be used during pregnancy and breastfeeding
- Trimethoprim / Cotrimoxazole: InfectoTrimet® / Cotrim, Bactrim®, Eusaprim®, Kepinol® => In certain regions, however, unfortunately many pathogens are already resistant to this antibiotic
My experiences: Despite all these recommendations for antibiotic administration, far too many sufferers still go home after their doctor's visit with the following:
- Without a urine culture (no pathogen determination and no sensitivity analysis for antibiotics)
- Fluoroquinolone antibiotic or a single dose of Fosfomycin
My truly sincere tip:
- Be persistent! Don’t let them fob you off, demand a urine culture with an antibiogram!
- No -floxacin antibiotics! Accept a fluoroquinolone antibiotic only if there is no other choice (according to the antibiogram).
- Single dose with emergency dose: Ask for a second single dose if the symptoms are not noticeably reduced three days after taking the first dose
Here is an overview table for the recommended empirical short-term antibiotic therapy for uncomplicated cystitis in women of premenopausal age: S3 Guidelines: Uncomplicated Urinary Tract Infections
What to Do if You Have a Urinary Tract Infection (UTI)
When you have a urinary tract infection (UTI), it's essential to take the right antibiotics to ensure that the infection is fully cleared and doesn't recur. Here are some tips on what to do if you suspect you have a UTI:
Don't Take Any Antibiotics You Have at Home
- Only take antibiotics that your doctor has prescribed for you.
- A urine sample can only be taken after the last antibiotic intake, which is usually 3-5 days. Wait until then before visiting your doctor's surgery to provide a urine sample.
Tell Your Doctor You Want a Urine Test and Antibiotic Sensitivity Report
- When you visit your doctor, ask them to take a urine sample from you. This will help determine which antibiotics are most effective against the bacteria causing your UTI.
- Tell your doctor that you want an antibiotic sensitivity report (antibiogram). This is essential in finding out which antibiotics work best for your specific infection.
Ask Your Doctor About a Backup Antibiotic for Emergencies
- In case of an emergency, ask your doctor to prescribe a standard UTI antibiotic that you can take at home. Ensure this is not a fluoroquinolone.
- Request a second pack if the prescribed antibiotic is a single-dose one (like Fosfomycin). This can be helpful in cases where one dose may not be enough to clear the infection completely.
Follow Your Doctor's Instructions
- If you're prescribed an antibiotic, make sure you complete the full course as directed by your doctor. Don't stop taking it unless advised to do so by a medical professional.
- If you experience symptoms despite completing the antibiotic course, consider consulting another doctor or specialist who can help identify why the infection persists.
No! And that's for many reasons:
- Spectrum of action: Not every antibiotic works against every germ. Some antibiotics are naturally resistant, i.e., they cannot affect the bacterial strain by nature. For example, Proteus mirabilis and Pseudomonas aeruginosa are naturally resistant to nitrofurantoin.
- Individual risk: Existing allergies, intolerances, interactions with medications or contraindications (e.g. during pregnancy).
- Sensitivity: How many percent of the germs in the bacterial strain are sensitive to the antibiotic, how many are already resistant?
- Eradication rate: How many percent of the germs are killed by a standard dose of the antibiotic - i.e., how effective is the substance?
- Collateral damage: What is the risk of developing multi-resistant bacteria or Clostridium difficile-associated colitis?
- Antibiotic stewardship: Rational and responsible use of antibiotics => for a uncomplicated infection, no reserve antibiotic should be used!
You might also want to read the answers to:
What is the best antibiotic for cystitis?
Which antibiotics are taken for acute cystitis?
If you're still interested in Basics, Do's & Don'ts when selecting antibiotics, I can recommend the presentation "The 1x1 of ANTIBIOTIC THERAPY" from the LKH Universitätsklinikum Graz.
All substances that fight bacteria are considered antibiotics (AB) or antibacterial chemotherapeutics. Antibiotics were originally synthesised by microorganisms, such as penicillins, cephalosporins, aminoglycosides. Antibacterial chemotherapeutics are synthetically produced by humans, e.g. sulfonamides, metronidazole, quinolones. In a broader sense, however, antibiotics (AB) are the common term.
There are now 160 active ingredients (often chemically modified and no longer derived from natural substances like fungi) that have an antibiotic effect.
Antibiotics always work only on the pathogens of the disease, not on the inflammation (disease) itself. However, the inflammation heals because there are no pathogens left to trigger inflammatory reactions in the tissue.
Depending on their antibacterial effectiveness, an antibiotic can be classified into one of two groups:
- Bactericidal: These antibiotics inhibit growth and kill bacteria (penicillins, cephalosporins, carbapenems, fluoroquinolones, aminoglycosides, glycopeptides, metronidazole, fosfomycin).
- Bacteriostatic: These antibiotics inhibit bacterial reproduction. Dormant bacteria cannot be killed by them (macrolides, tetracyclines like doxycycline, clindamycin, linezolid, nitrofurantoin).
Antibiotics can also be classified by their mechanism of action:
- Inhibition of cell wall synthesis: Beta-lactam antibiotics (penicillins, cephalosporins, monobactams, carbapenems), glycopeptide antibiotics (vancomycin, teicoplanin, telavancin, dalbavancin), fosfomycin
- Nucleic acid metabolism (interference with bacterial DNA or RNA): Fluoroquinolones/quinolones (norfloxacin: reaches sufficient levels only in the urine, ofloxacin, ciprofloxacin, levofloxacin, moxifloxacin), nitroimidazole derivatives (metronidazole, nitrofurantoin), rifampicin
- Inhibition of bacterial protein synthesis: Macrolides (roxithromycin, clarithromycin, azithromycin), tetracyclines (doxycycline), aminoglycosides (gentamicin, amikacin), etc.
- Interference with tetrahydrofolic acid synthesis: Sulfonamides, trimethoprim => combined as cotrimoxazole (sulfamethoxazole + trimethoprim)
In addition to the antibacterial activity, the spectrum of activity of the substance is crucial:
- Narrow-spectrum antibiotics: These antibiotics target only a few gram-positive or gram-negative pathogens.
-
Broad-spectrum antibiotics:
These antibiotics target multiple pathogens with their mechanism of action, covering a "broad spectrum" of bacteria.
These include:
- Aminopenicillins
- Cephalosporins
- Fluoroquinolones
- Carbapenems
If you'd like to know more details about the individual substances, I recommend the following page: "Antibiotics Overview" by AMBOSS
The Problem with Resistances
Bacteria manage to outsmart antibiotics and ensure their survival through several mechanisms (e.g. they produce enzymes that render antibiotics ineffective or alter metabolic pathways that antibiotics would otherwise block, etc.).
Thanks to these mechanisms, entire bacterial strains become resistant to antibiotics. This happens more easily the more frequently bacteria come into contact with antibiotics (so the risk increases with each use). Bacteria can even transfer their resistance mechanisms from one bacterial species to another, resulting in the emergence of multiresistant strains that are resistant to multiple antibiotics at once.
Not every antibiotic fights all bacteria equally well. Some substances only kill a few types of bacteria (narrow-spectrum antibiotics), while others work against a wide range of bacteria simultaneously (broad-spectrum antibiotics or broad-spectrum antibiotics). Whenever possible, narrow-spectrum antibiotics should be used, as this leads to fewer resistances and fewer side effects. However, the bacteria (or bacteria) must first be identified through a bacterial culture. Only then can the "best antibiotic" be selected after the identified bacteria have undergone resistance testing (antibiogram).
In the case of severe infections or when there is a risk of an unfavourable course of the illness, it may still be reasonable to start treatment immediately with a broad-spectrum antibiotic after requesting a bacterial culture, as experience shows it is effective => empirical/calculated therapy. Once the result of the antibiogram is available after a few days, a switch to a suitable narrow-spectrum antibiotic can then be made.
The S3 guidelines provide clear recommendations on the selection, dosage, and duration of therapy.
Following the guidelines, the calculated/empirical short-term therapy should be preferred, especially for women in the premenopausal phase.
The short-term therapy (3 to 5 days) is preferred over the conventional therapy (7 to 10 days) for the following reasons:
- Better patient adherence (= adherence to the therapy)
- Fewer side effects (side effects = unwanted drug effects)
- Less resistance development: Lower selective pressure for resistant pathogens from the periurethral, vaginal, and fecal flora
As long as necessary, as short as possible!
For many years, it was believed that longer antibiotic therapies reduced the likelihood of infection recurrence or the development of resistance.
The still widely held belief: "Finish the pack". However, it is now known that such a simple rule is not sufficient for modern antibiotic therapy.
Today we know: the longer bacteria are exposed to the selective pressure of an antibiotic, the more likely it is that mainly resistant, i.e., antibiotic-insensitive pathogens, will survive.
Increasingly, studies show that for various infections, shorter antibiotic therapies are equivalent or even superior to longer therapies. A shorter antibiotic therapy not only has the advantage of fewer resistance developments but also leads to fewer side effects.
Another point we should be aware of: Underdosing leads to therapy failure . The dosage recommendations in the package insert usually follow a standard formula. For example, a woman weighing 56 kg and measuring 1.50 m is recommended the same dose as a man who is 1.90 m tall and weighs 90 kg.
In the future, the rule for antibiotics should be:
"The treatment should be as short as possible, but as long as necessary."
However, implementing this new credo is unfortunately not so straightforward:
- How long is "as long as necessary"?
- And what dosage is "as much as necessary"?
This depends on many factors, and there is no one-size-fits-all solution.
Duration of Therapy
The length of time an antibiotic needs to be taken depends on several factors, including:
- Type of the disease
- Severity of the disease
- Individual progression of the disease
- Triggering bacterial type
- Active substance of the antibiotic (for example, Nitrofurantoin 5-7 days, Trimethoprim 5-7 days)
Dosage
According to the recommendations of EUCAST (European Committee on Antimicrobial Susceptibility Testing), there are sufficient guidelines for adult dosage in clinical practice (both standard and high daily dosage).
The dosage of an antibiotic depends on several other factors, such as:
- Body weight: unusually high or low body weight
- Body composition: ratio of fat to muscle mass - adipose tissue influences the effect of a drug
- Organ health: breakdown of active substances by the liver and kidneys
The Big Danger: Under-dosing over a prolonged period
Most pathogens become resistant to antibiotics because the dosing is not high enough to eliminate as many/all germs as possible in the first step.
Some antibiotics develop resistance very quickly - aminopenicillins, cephalosporins, and macrolides. Low drug levels over a prolonged period likely play a major role in the development of resistance.
For example, the active ingredient of the macrolide antibiotic Azithromycin is measurable in plasma for a long time after the therapy ends. The consequence: In half of the patients who had received Azithromycin, scientists found erythromycin-resistant Streptococcus pneumoniae.
Conclusion: A few basics
I am convinced that it is really challenging to choose the best possible antibiotic therapy. It requires:
- Individual approach
- Comprehensive knowledge of optimal therapy for various conditions
- More precise monitoring of the respective disease progression
So basically, a medical expert with plenty of time for patients.
And although I am neither a doctor nor an expert, I would like to share with you a few thoughts that I "wrote behind my ears" after my thorough research.
- First, take a urine culture + antibiogram, then the antibiotic!
- Tips for the urine sample for the urine culture: First morning urine, the last bladder emptying should be more than 4 hours ago, before any antibiotic intake, immediately sent to the laboratory (or stored at 2-8°C)
- Targeted therapy is always better! A diagnostic test using urine culture and antibiogram clears many questions at once: Which antibiotics are sensitive?
- Calculated/Empirical therapy: Fosfomycin-trometamol, nitrofurantoin, and pivmecillinam have low resistance rates. Trimethoprim and cotrimoxazole have high resistance rates. No -floxacin antibiotics (fluoroquinolones)! More on this under Which is the best antibiotic for bladder infections?
- Dosing: sufficiently high (especially in cases of overweight). Kidney function should be monitored: Risk of under-dosing when adjusting the dose due to kidney insufficiency. Here you will find a reference table with standard dosing and high dosing: Resistance testing and antibiotic dosing
- Duration of therapy: a difficult topic... too long promotes resistance, too short may not eliminate all pathogens and promotes, for example, recurrent bladder infections.
- Therapy frequency: The pathogen sensitivity decreases as antibiotic use increases. This means the more frequently you take an antibiotic, the higher the risk of developing (multi)resistant pathogens.
A mixed infection refers to an infection with two or more organisms occurring simultaneously.
In a routine antibiogram**, a sensitivity test is usually performed for all the organisms found in the urine culture. You can find an example of a bacteriological report from a mixed infection with two organisms at this link.
The antibiotics that are effective against all the organisms involved in the infection should be used. This is known as a polymicrobial infection**. The choice of antibiotic will depend on the organisms present and their sensitivity patterns. Your healthcare professional will advise on the best course of treatment.
It's worth noting that Enterococcus faecalis, also known as Enterococcus faecium, are often found in mixed infections. However, whether these bacteria are pathogenic or not is still unclear. You can find more information about this at this link.
To prevent contamination, the urine sample should be handled correctly. You can find more information about this at this link. A further option to ensure that the sample is not contaminated during collection is to use a catheter to collect urine directly from the bladder.
Quick processing of the sample is also essential. It should be sent to the laboratory or stored at 2-8°C** as soon as possible. Bacteria can multiply quickly at room temperature and therefore contaminate the sample, affecting the test results. An example showing how quickly the bacterial count can increase over time can be found at this link.
Why is a Urine Culture done?
A Urine Test Strip (a rapid test) is a good way to determine if a urinary tract infection (UTI) is likely. Elevated leukocytes and/or erythrocytes indicate inflammation, nitrite suggests a nitrite-producing bacterial infection (E. coli, Klebsiella, Proteus Mirabilis).
If there is suspicion of a UTI, it is always beneficial to determine the causative organism (bacteria, fungus) - and that's exactly what a urine culture in a laboratory does.
If bacteria are found in the urine culture, the sensitivity/resistance against antibiotics is usually also determined - a so-called Antibiogram. The result of the Antibiogram shows which antibiotics can be used against the bacteria found in the urine culture.
The ideal sequence from symptom onset to antibiotic administration:
- Urine Test Strip => Suspicion of UTI
- Urine Culture => Determine causative organism and sensitivity/resistance against antibiotics
- Antibiotics => Administered based on Antibiogram results
The bacterial count is measured in CFU (colony-forming units). A colony on the plate (=culture medium) represents one CFU in the urine. It is counted exactly, and from a count of 100, it is estimated or compared to exact reference images. The count is always rounded up to the nearest ten. Depending on the volume of urine placed on the plate, the count is then multiplied by CFU/ml.
Generally, a bacterial count of 10^5 CFU/ml (100,000 CFU/ml) or more is considered significant and indicates a urinary tract infection. However, in the following cases, a bacterial count of less than 10^3 (1,000 CFU/ml) may also be an unambiguous sign of a clinically significant UTI:
- Clear symptoms of a UTI and/or leukocytes or nitrite in the urine
- Presence of antibacterial substances (positive inhibition test) in the urine
- In bacteria that generally do not multiply well in the urine, such as Staphylococcus saprophyticus
- At a short duration of urine retention (sample collection too quickly after bladder emptying)
- In cases of increased urination (excessive fluid intake, diuretic use, abnormal increased urination)
- With nephritis or kidney abscess
- In children's urine
- With biofilm formation => most bacterial cells are attached (growing on the surface) and only a few are planktonic in the urine
- In bacteria embedded in the bladder mucosa => only a few are planktonic in the urine
Firstly, it's essential to determine whether you have a complicated or uncomplicated UTI. Complicated UTIs are often associated with symptoms like fever, chills, or a severe burning sensation during urination. In these cases, antibiotics should not be delayed until the urine culture results are available.
Instead, a broad-spectrum antibiotic is usually prescribed immediately to cover possible pathogens and to start treating the infection promptly.
General Principles
- In uncomplicated UTIs (without fever or blood in urine), it's recommended to perform a urinalysis before starting antibiotics.
- Before prescribing an antibiotic, the clinician should consider the following factors: • The severity of symptoms • Past medical history, including allergies and sensitivity to specific antibiotics • Pregnancy status (if applicable) • Any relevant comorbidities or complications
General Antibiotics for UTI
The general choice of antibiotic should cover the most common pathogens, such as E. coli, Proteus mirabilis, and others.
What antibiotics are commonly used for UTI?Specific Antibiotics for UTI
For complicated UTIs or those with fever and blood in urine, more specific antibiotics may be chosen based on the urinalysis results.
What are some common antibiotics for uncomplicated and complicated UTI?General Antibiotics
The general choice of antibiotic should cover the most common pathogens, such as E. coli, Proteus mirabilis, and others.
What antibiotics are commonly used for UTI?An antibiogram is used in a microbiological laboratory to test which antibiotics are effective against the pathogen(s) found in the urine culture.
Why perform an Antibiogram?
The antibiogram is helpful because no antibiotic is effective against all possible pathogens. Not only because not every antibiotic works against every pathogen (natural resistance), but also and especially in times of increasing multi-resistance, it is more important than ever to handle antibiotic therapy carefully.
Unfortunately, the current practice is often as follows: One antibiotic after another is prescribed until one is found that works. This uncritical use of antibiotics unnecessarily harms the microbiome and promotes resistant pathogens.
How is an Antibiogram performed?
The starting point for the antibiogram is a detected pathogen. In the case of bladder infections, the pathogen(s) are usually identified in a urine culture.
There are two different methods for performing the antibiogram:
- Agar diffusion test
- Dilution method
In the agar diffusion test, the pathogen to be tested is spread over a plate with a nutrient medium. The plate is then covered with circular discs containing various antibiotics in defined amounts. During incubation, the pathogens grow towards the disc until a concentration of the antibiotic is reached that is sufficient to inhibit growth, creating a so-called inhibition zone around the disc. Each antibiotic has outer and inner target inhibition zone sizes. If the measured inhibition zone is:
- outside the outer target value, the pathogen is sensitive (S)
- within the inner target value, the pathogen is resistant (R)
- between the outer and inner target limits, the pathogen is classified as intermediate (I)
The larger the inhibition zone, the more sensitive the pathogen is!
In the dilution method, a more precise approach is used to determine the Minimum Inhibitory Concentration (MIC) for various antibiotics against the identified pathogen.
The MIC is the smallest concentration of an antimicrobial substance (e.g. an antibiotic) that still prevents the pathogen from growing in the culture.
In the microdilution method, the pathogen is mixed with a defined amount of an antibiotic in a liquid nutrient medium in a microtiter plate.
A dilution series with different concentrations of the antibiotic is performed (1, 2, 4, 8, 16, 32 mg/L).
The growth of the microorganism is indicated by a cloudiness in the nutrient medium.
The mixture with the lowest concentration of the antibiotic where the liquid remains clear provides the MIC value.
The smaller the MIC, the more sensitive the pathogen is!
How is an Antibiogram interpreted?
Depending on the method, the result for each tested antimicrobial substance will either be Sensitive (S), Intermediate (I), and Resistant (R), or the Minimum Inhibitory Concentration (MIC) + interpretation of S-I-R.
S-I-R is interpreted as follows:
- S = Sensitive => high probability of therapeutic success with standard dosage
- I = Sensitive with dosage recommendation => high probability of therapeutic success with increased exposure through an adjusted dosage regimen or through concentration at the infection site
- R = Resistant => high probability of therapy failure
You can find the dosage tables for standard and high dosages at the National Antibiotic Sensitivity Testing Committee (NAK) under Resistance Testing and Antibiotic Dosage.
To illustrate, here is an example of an antibiogram for a mixed infection with two pathogens.

The standard dosage for Amoxicillin/Clavulanic acid for uncomplicated UTIs (excerpt from the NAK reference table): 3 x daily 0.5 g Amoxicillin + 0.125 g Clavulanic acid, oral.
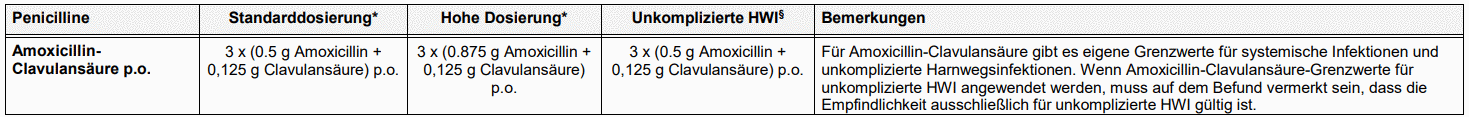
The presence of three or more potentially uropathogenic bacterial strains is most likely due to contamination. In such cases, no resistance determinations are made and the submission of a sterile urine sample is recommended.
In particular, when mid-stream urine is collected, contaminating bacteria are often found due to incorrect collection. Urine is a (nearly) sterile bodily fluid. However, as the anterior urethra is physiologically colonised with bacteria, contamination can occur during urine collection. The most common contaminants include:
- coagulase-negative Staphylococci (except S. saprophyticus)
- greening Streptococci
- Enterococci: often after antibiotic therapy
- Coryneform bacteria
- Propionibacterium
- Lactobacillus sp.
- Candida (fungi): often after antibiotic therapy
To help you get into this topic, I recommend reading the article: How do you know which antibiotic works?
Trap #1: The bacteria are resistant => The antibiotic can't work at all
After reading the article, one key point will have stuck with you: An antibiotic treatment without knowing the causative pathogen always carries the risk of being unsuccessful.
- The pathogen may be naturally resistant to the antibiotic. For example, Mycoplasma bacteria have no cell wall and are therefore resistant to β-lactam antibiotics (all cell wall synthesis inhibitors, including Fosfomycin).
- The pathogen may have already developed a resistance to the antibiotic.
The solution: Urine culture + Antibiogram. In my view, it is essential that a culture is taken from your urine to identify the pathogen(s) before the first dose of antibiotics is administered. The antibiogram will clearly show which antibiotics are effective against your pathogen(s). You can view an example of such a result here: Example of a bacteriological report of a mixed infection with two pathogens.
Trap #2: Too low a dose and/or too short a therapy
The symptoms improve slightly, but the UTI doesn't heal completely. Too many pathogens remain (possibly now with more resistance mechanisms) and after a few days or weeks, the inflammation flares up again. Although short-term therapy (single dose or 3 days) is often preferred, I'm not particularly fond of it. Even less so am I a fan of insufficient dosages, as this promotes resistance - the pathogens have far too much room to develop resistance under the selective pressure.
Conclusion: It's better to shoot with a targeted cannon, and put the shotgun aside.
The very commonly prescribed classic in Trap #2: The antibiotic Fosfomycin as a single dose (Monuril®). Fosfomycin is a good active ingredient and, moreover, a reserve antibiotic, but a single dose is often insufficient to overcome the pathogen load. According to a study comparing it with Nitrofurantoin, nearly half of the participants were still not symptom-free 28 days after the end of therapy.
The solution: No single dose (or at least another single dose after three days), therapy duration at least 5 days, better a higher dose (if individual circumstances allow) than underdosing.
Trap #3: The pathogens are hiding
Bacteria unfortunately always find ways to protect themselves from an antibiotic attack. Especially with UTIs, there are two ways in which the pathogens hide:
- In the biofilm: Bacterial colonies are protected by a self-produced extracellular polymeric matrix, the biofilm.
- In the urothelium (embedded pathogens): Intracellular bacterial communities => Uropathogenic bacteria can also invade the urothelial cell and form a biofilm-like community there. This protects the bacteria from the immune system, is the trigger for recurring UTIs, and can cause symptoms even when standard diagnostics can't detect a UTI.
In the biofilm and urothelium, bacteria survive up to 1,500 times higher antibiotic concentrations.
Learn more on the topic at Is a UTI always detectable in urine?
The solution to this problem is unfortunately not simple, and there are various approaches, with differing levels of testing and reliability:
- Forskolin* to eliminate intracellular bacteria. Alternatively, Chitosan* acts as a bladder wall exfoliant (removing the superficial layer of bladder cells).
-
Biofilm inhibitors:
- Phytopharmaceuticals: For example, nasturtium and horseradish ( Angocin® Anti-Infekt N* ), arbutin (from bearberry leaves), coumarins.
- N-Acetyl L-Cysteine (NAC): Antioxidative, anti-inflammatory, and mucolytic (mucus-dissolving); destroys and reduces biofilm formation by bacteria and fungi.
- Lactoferrin: The enzyme lactoferrin deprives bacteria of essential nutrients like iron, preventing biofilm formation as bacteria continually search for nutrients. Lactoferrin is a natural peptide found in tears, saliva, and breast milk.
- Enzymes (e.g. nattokinase, serrapeptase): Interfase® Plus - Klaire Labs, Biofilm Defense® - Kirkman®
- Long-term antibiotic therapy in combination with the urinary tract disinfectant Hiprex® (e.g. in the private clinic at Harley Street 10 in London).
- Phage therapy: Phages are viruses that attack and dissolve bacteria (including in biofilms and dormant bacteria called persisters). Phage therapy is still practiced in countries of the former Eastern Bloc. Phages are host-specific, meaning they target a specific bacterial species.
Trap #4: It’s Something Else
If there are no typical uropathogenic bacteria colonizing you, then (standard) antibiotics can do little to help. Sometimes, rare pathogens (often sexually transmitted) require special detection methods (e.g. PCR, microscopy), such as:
- Infection with sexually transmitted bacteria: Gonococci, chlamydia, mycoplasma, ureaplasma, trichomonas (protozoa). They often cause symptoms in the urethra => urethritis (inflammation of the urethra).
- Infection with fungi: Usually candida species but also aspergillus => Detection through microscopic urine examination.
- Infection with parasites: Urogenital schistosomiasis (bilharziasis) => Microscopic detection of schistosomes.
- Infection with rare pathogens: Non-tuberculous mycobacteria, anaerobes (Peptococcus and Peptostreptococcus), Gardnerella vaginalis
- Infection with viruses: The herpes simplex virus can infect the urethra, cause pain during urination, and lead to problems emptying the bladder. . A BK (polyoma) virus infection can lead to cystitis with visible blood in the urine, particularly in immunosuppressed patients.
Not all cases of pain, burning, or frequent urination are caused by bacterial inflammation.
- Obstructions: Bladder stones, kidney stones, urethral diverticula, tumours (bladder cancer).
- Endometriosis: A painful condition where uterine lining tissue (endometrium) grows outside the uterus (e.g. on the ovary or bladder).
- Vaginitis: Vaginal inflammation can cause symptoms similar to cystitis.
- Vulvovaginitis: Inflammation of the female external genitalia, including the vagina.
- Vulvodynia / Vestibulodynia: Itching, burning, stinging, dryness, soreness, or pain in the external female genital area. Sometimes also affecting vaginal, pelvic floor, or anal areas.
- Salpingitis: Inflammation of the fallopian tube.
- Overactive bladder (OAB): Chronic irritation of the lower urinary tract, causing symptoms similar to a UTI (frequent and painful urination), but urine tests show no abnormalities. Symptoms are typically less severe at night.
- Radiation: Bladder inflammation following radiotherapy.
- Mechanical or chemical irritation: For example, due to bladder catheters, medications (painkillers, chemotherapy).
- Urinary retention issues: Mechanical bladder emptying obstruction (e.g. urinary tract blockages, urethral stricture), neurogenic bladder emptying issues (nerve damage in the brain or spinal cord).
- Pelvic organ prolapse (bladder prolapse): Impaired bladder function (incontinence, residual urine), increased susceptibility to bladder infections.
- Musculoskeletal and connective tissue disorders: Pelvic floor hypertonicity, lumbar spine disc problems, etc.
- Gastrointestinal disorders: Irritable bowel syndrome, leaky gut, etc.
- Interstitial cystitis / Bladder Pain Syndrome (IC/BPS): A non-infectious, chronic bladder condition with symptoms resembling bladder infections. The exact cause is unclear, making IC/BPS a diagnosis of exclusion. Due to damage in the bladder’s protective lining, irritating substances from urine penetrate deeper layers of the bladder wall, causing inflammation.
- Histaminosis (mast cell activation syndrome MCAS, histamine intolerance): Excess histamine due to overactive immune defense of mast cells in MCAS, or a metabolic disorder in histamine intolerance, can lead to chronic bladder inflammation.
The solution: Don’t give up and keep searching. Be sure to have everything thoroughly checked gynaecologically. Consider and rule out all differential diagnoses. I know of several cases where urologists unsuccessfully treated chronic bladder infections for years, only for a gynaecologist to discover the root cause was endometriosis.
Conclusion: Use antibiotics carefully & think outside the box
What certainly doesn’t help (apart from creating more resistant bacteria):
Trying one antibiotic after another in the hope that the nth one will work.
Even the perfectly matched antibiotic can only successfully combat the bacteria if it is used correctly.
Consistent active ingredient levels are crucial
It is important to take the medication as prescribed, because only then will there be a sufficiently high concentration of the active ingredient in the body to eliminate the pathogens. If the antibiotic cannot fully develop its effect (e.g. due to inaccurate intake or premature discontinuation), the therapy may fail. And the much worse consequence: resistant bacteria may survive and become resistant to the antibiotic.
-
Correct timing: Three times daily does not mean upon waking, at lunch, and at dinner.
- 1x daily: Take the tablet (prescribed dose) approximately every 24 hours, e.g. always in the morning at the same time.
- 2x daily: Take the tablet about 12 hours apart, e.g. one at 8:00 a.m. and one at 8:00 p.m.
- 3x daily: Take the tablet about every 8 hours, e.g. the first dose at 7:00 a.m., the second dose after lunch at 3:00 p.m., the third dose before bedtime at the earliest 10:00 p.m.
- Correct dosage: Caution! Some antibiotics (e.g. doxycycline) are given at higher doses at the start of treatment to quickly reach the required active ingredient concentrations.
- Do NOT take with milk, tea, coffee, antacids, mineral supplements (calcium, magnesium, or zinc): Taking these at the same time as antibiotics can hinder the absorption of the active ingredient in the stomach.
- Plenty of water: Take with a large glass of water - not just a sip! Otherwise, there is a risk of the medication getting stuck in the oesophagus, which can even damage the tissue.
- Not lying down immediately: Tablets can adhere to the oesophagus when lying down and damage the tissue there. Always follow the package insert instructions, e.g. do not lie down for 1–2 hours after taking doxycycline.
-
Follow package insert instructions: Manufacturers provide detailed instructions in the package leaflet, which should be strictly followed, such as:
- Before meals: Take the tablet half an hour to one hour beforehand (reason: Some active ingredients are less well absorbed if taken with food).
- With meals: Take the tablet directly with a meal.
- Interaction check: Some antibiotics have potentially dangerous interactions with other medications, e.g. macrolide antibiotics (erythromycin, etc.) and cholesterol-lowering drugs (statins) - the statin's effect is enhanced. Other examples: blood sugar fluctuations in people with diabetes, increased bleeding tendency, etc. A practical service from Apotheken Umschau is the Interaction Check, where you can easily check if your medications have interactions.
-
Adherence to therapy:
- Don’t forget: Set reminders in your smartphone calendar or use dedicated apps. Should you skip or make up for missed medication? This depends on the active ingredient.
- Don’t stop prematurely: Even if symptoms improve, treatment should never be stopped without consulting a doctor.
- Fear of side effects: The package leaflet must list all known side effects; however, not every patient will experience them. Learn how to interpret side effects from the leaflet in an article from Apotheken Umschau: Side Effects: What You Should Know.
Stopping antibiotics prematurely can lead to the worsening of the infection. When symptoms subside, the bacterial cultures may only have been reduced, leaving enough pathogens in the body for a relapse. This can result in a recurrence, particularly in cases of a weakened immune system.
However: The course of the illness and the severity of a UTI are very individual. While some experience symptom relief the day after starting treatment, others may endure symptoms for several days.
Basic rule: Follow the prescription
The basic rule for taking antibiotics is to follow the prescription:
- Take them for the prescribed duration, even if symptoms improve.
- Do not take less than the recommended dose.
- Follow instructions for use: What should I keep in mind when taking antibiotics?
- No improvement? => Contact your doctor.
-
Experiencing side effects? => Consult your doctor before stopping the medication. Typical side effects include:
- Itching
- Rash
- Swelling
- Muscle and tendon pain
My advice: If you feel the antibiotic is not working, or if symptoms persist towards the end of the treatment (e.g. after a single dose of fosfomycin or a 3-day course), contact your doctor immediately. You may need a different antibiotic or an extended treatment duration.
Not every side effect is a true allergy
An estimated four out of five reactions to a medication are not allergic but rather "normal" side effects. Never stop taking medication on your own, even if you feel it’s not effective or if there are too many side effects - always consult a doctor. They can determine if it's truly an allergy and, if necessary, provide an alternative medication.
Caution: Some people do have true allergic reactions to certain antibiotics. Allergies to antibiotics like penicillin are the most well-known. Severe allergic reactions can, in rare cases, cause life-threatening breathing or cardiovascular problems. If you suspect an allergy, seek medical attention immediately. In most cases, alternative drug classes are available.
Stopping early does not necessarily lead to resistance
As with any other medication, the rule for taking antibiotics is: as short as possible, but as long as necessary.
The widespread assumption that stopping antibiotics too early generally creates more resistant bacteria (compared to completing the entire course) is, according to studies from England, scientifically unproven. (Note: Certain bacterial strains and medications may be exceptions, e.g. with tuberculosis, pathogens can develop resistance due to stopping therapy early).
The majority of resistance develops through so-called "collateral selection". Everyday bacteria, which usually do not cause illnesses, develop resistance through long-term antibiotic treatment and can thus become a threat to the affected person.
Selection, dosage, and duration of therapy
The S3 Guideline provides clear recommendations regarding selection, dosage, and duration of therapy: Which antibiotics are used for acute bladder infections?
For premenopausal women, empirical short-term therapy (3-5 days) is recommended. Ultimately, the treating doctor decides on the optimal duration of intake, tailored specifically to the infection and the expected course.
In this FAQ, you can read about the advantages and disadvantages of shorter or longer antibiotic treatments: What is better? A short-term therapy (3-5 days) or a standard therapy (5-10 days) with antibiotics?
In Germany, Austria, and Switzerland, antibiotics are subject to a prescription requirement (also known as a prescription-only medication). This means in practice that antibiotics are not available over-the-counter and a prescription is always required.
Some online services for getting antibiotics are much more expensive than the classic visit to the doctor/GP. Online portals also do not take a urine culture, so they can only initiate a calculated therapy with antibiotics based on a questionnaire. For me, this means that I am not convinced of the necessity 100%. It is probably always better to find a GP who initiates treatment...
Nitrofuran derivative Furazidin
The antibacterial Furazidin is available over-the-counter in Poland and has a similar mechanism of action to Nitrofurantoin. It acts against both gram-positive (Staphylococcus epidermidis, Staphylococcus aureus, Staphylococcus faecalis) and gram-negative microorganisms (Enterobacteriaceae – Salmonella, Shygella, Proteus, Klebsiella, Escherichia, Enterobacter etc.). It is used to treat urinary tract infections.
My conclusion
Online services for getting antibiotics are much more expensive than the classic visit to the doctor/GP. Also, online portals do not take a urine culture and can only initiate a calculated therapy with antibiotics based on a questionnaire. For me, this means that I am not convinced of the necessity 100%.
Antibiotics Natural antibioticsAll antibiotics have side effects, and any antibiotic can rarely cause severe side effects.
The key difference in this context is: how often do severe side effects occur, and are they reversible?
Floxed!
A group of antibiotics unfortunately still popular for urinary tract infections is the fluoroquinolones. This includes substances ending with -floxacin, such as ciprofloxacin, levofloxacin, moxifloxacin, norfloxacin, and ofloxacin. Despite this, a Red Hand Letter was issued in 2019 regarding the use of fluoroquinolone antibiotics.
The reason: Severe and persistent side effects that impact quality of life and may be irreversible, mainly affecting the musculoskeletal system and nervous system.
Recommendations:
- Not for uncomplicated cystitis
- Not for recurrent lower urinary tract infections
The only exception: If all other antibiotics usually recommended for these infections are deemed unsuitable. And even then, never in combination with corticosteroids.
What does this mean for you?
You should always refuse fluoroquinolone antibiotics unless there is no alternative, which is very rarely the case.
If you must take fluoroquinolone antibiotics, you should immediately stop the treatment at the first signs of these severe side effects:
Severe side effects affecting the musculoskeletal system include:
- Tendinitis (tendon inflammation) and tendon rupture
- Myalgia (muscle pain), muscle weakness
- Arthralgia (joint pain), joint swelling
- Gait disturbance
Severe side effects affecting the peripheral and central nervous system include:
- Peripheral neuropathy (various nerve damages): sensory disturbances, abnormal sensations such as tingling, burning, or "pins and needles", disturbances in touch, pain, or temperature sensitivity, etc.
- Insomnia
- Depression
- Fatigue
- Impaired memory
- Visual, auditory, olfactory, and taste disturbances
Conclusion
For a long time, I was also unaware of the issue. I consider myself lucky that the antibiotics like Cipro and others never caused severe side effects for me. Unfortunately, through support groups, I know of numerous cases where people suddenly can hardly walk or experience severe neurological impairments.
Yet many doctors routinely prescribe these medications for minor infections. It’s incomprehensible – because fluoroquinolones should really only be used for more serious infections, when no alternatives are available.
WARNING! The most common interactions with other medications
- Statins (=cholesterol-lowering drugs) and macrolides: The interaction between macrolides (roxithromycin, clarithromycin, azithromycin) and statins is classified as severe. There is a risk of myopathies (muscle disorders) and rhabdomyolysis (breakdown of muscle fibres). Macrolides are used for infections caused by pathogens such as chlamydia, mycoplasma, streptococci, and gonococci.
- Antiarrhythmics and fluoroquinolones: When fluoroquinolones are combined with other QT interval-prolonging drugs, such as antiarrhythmics of classes IA and III (medications for heart rhythm disorders), there is an increased risk of cardiac arrhythmias (ventricular arrhythmias, torsades de pointes). Fluoroquinolones (all antibiotics ending with -floxacin) are often unnecessarily prescribed for UTIs. Macrolides can also prolong the QT interval in the ECG, so caution is also required when macrolides and antiarrhythmics are taken together.
- NSAIDs (e.g. IBU) and fluoroquinolones: When non-steroidal anti-inflammatory drugs (NSAIDs) (except acetylsalicylic acid) are taken together with fluoroquinolones, significant, clinically relevant interactions occur => NSAIDs amplify the neurotoxic side effects of fluoroquinolones by up to 300 times. So: Do not take NSAIDs such as ibuprofen/diclofenac together with fluoroquinolones (all antibiotics ending with -floxacin)!
A great article on toxic effects: Toxic effects of selected antibiotics
Gastrointestinal issues
Antibiotics do not differentiate between harmful and beneficial bacteria; they affect all bacteria in the human body within their spectrum of activity. Thus, they destroy not only the culprits (e.g. E. coli in the urinary tract) but also the beneficial bacteria in the gut and vagina. The result is often a bacterial imbalance – a disrupted microbiome.
An antibiotic-induced gut flora disruption often manifests as diarrhoea, stomach pain, and nausea. In cases of bloody diarrhoea or severe abdominal pain, it could indicate a life-threatening inflammation of the colon (pseudomembranous colitis), caused by antibiotic-associated overgrowth of Clostridium difficile.
Countermeasure: Probiotics: For bloody, slimy, or cramping diarrhoea, return to your doctor immediately.
For mild diarrhoea, you can counteract with probiotic products even during antibiotic treatment.
Probiotics aim to repopulate the beneficial bacteria in the gut.
Often, the gut recovers on its own, but sometimes diarrhoea persists despite probiotics. In such cases, I recommend a stool analysis.
The results will provide targeted recommendations for replacing the missing bacterial strains.
Fungal infections
An antibiotic-induced vaginal flora disruption often leads to fungal infections, sometimes with a delay of 1-2 weeks. Due to the drastic reduction of protective lactobacilli caused by antibiotics, pathogenic yeasts, most commonly Candida albicans, proliferate. A vaginal yeast infection (vaginal mycosis) increases the risk of a subsequent urinary tract infection, thus perpetuating the vicious cycle.
Countermeasure: Lactic acid and lactobacilli: A yeast infection is unpleasant, and its treatment further affects the vaginal flora. If you are prone to yeast infections, the motto should be: Prevention is better than cure!
- Only use lukewarm water for cleansing down under
- Wear breathable cotton underwear and avoid panty liners
- Preventatively use local treatments with lactic acid and lactobacilli alternately
Do you suspect a fungal infection?
- Ideally, visit your gynaecologist for a swab test
- Alternatively, an antifungal medication (vaginal suppositories and creams) from the pharmacy containing one of the following active ingredients: Clotrimazole, Miconazole, Nystatin
- Do not use products for vaginal restoration with lactic acid during fungal treatment!
- Only after fungal treatment rebuild the vaginal flora with lactic acid and lactobacilli alternately
Allergic reactions
According to specialists, only about 2-3% of the population truly suffer from an antibiotic allergy.
In the worst case, an allergic individual might experience an anaphylactic shock approximately 30 minutes after ingestion – causing a circulatory collapse and necessitating immediate hospitalisation.
However, reactions such as skin rash, redness, and itching are usually "just" a hypersensitivity reaction – an individual, unpredictable response to the antibiotic.
In any case of such overreactions, you should consult your treating doctor.
Often, the simplest solution is to switch to a different, effective antibiotic.
Tendonitis, nerve damage, and psychosis
These side effects can occur with the use of fluoroquinolone antibiotics.
Learn more at Which antibiotics have serious side effects?
Overview table
Maybe!
Antibiotics and their active substances have no direct or immediate effect on the efficacy of contraceptive pills (except for the TB antibiotic Rifabutin). However, here's the thing: Antibiotics have a very common and for some contraceptive pills fatal side effect - stomach and intestinal discomfort, i.e. vomiting and diarrhoea.
Especially broad-spectrum antibiotics destroy a large part of the bacteria flora in the gut. This often leads to diarrhoea. Diarrhoea means that the active ingredients of the pill are only reducedly absorbed, and therefore the contraceptive effect may not be guaranteed.
If you need to vomit within 3 hours after taking the pill, you can take it again within the next 12 hours. If you vomit multiple times, the protection for that month is not guaranteed.
Conclusion: If you don't experience vomiting or diarrhoea from the antibiotic intake, there's nothing to worry about. However, if you're unable to go to the loo or need to vomit (even if you're not taking antibiotics!), then use an additional method of contraception, such as a condom or diaphragm for that monthly cycle.
Pregnancy and breastfeeding are particularly sensitive periods during which medication should ideally be avoided. However, medically necessary medications, such as antibiotics for a bacterial infection, are exceptions. Untreated infections can harm the mother and sometimes the child.
Urinary tract infections during pregnancy must be treated, as there is a risk of kidney infection (pyelonephritis gravidarum) and associated preterm birth.
Which antibiotics can be used during pregnancy is best determined by your gynaecologist.
Typically, the following antibiotics are suitable for cystitis or pyelonephritis:
- Penicillins: Ampicillin, Amoxicillin (unfortunately, often ineffective due to resistant pathogens)
- Pivmecillinam: Narrow-spectrum penicillin, Selexid®, Pivmelam®, X-Systo®
- Macrolides: Azithromycin, Erythromycin
- Cephalosporins: Cefalexin, Cefuroxime, Cefuroxime, Cefixime, Cefadroxil (except Cefpodoxime)
- Fosfomycin: Second-choice medication, as there is limited information about its use during pregnancy.
The following antibiotics, often used for urinary tract conditions, are contraindicated (=not suitable) during pregnancy:
- Fluoroquinolones: Ciprofloxacin, Ofloxacin, Moxifloxacin, Norfloxacin, Levofloxacin
- Trimethoprim and Trimethoprim-Sulfamethoxazole (due to its effects on folic acid balance)
- Nitrofurantoin and its derivatives (especially not during the last three months before birth)
- Tetracyclines, such as Doxycycline (e.g. for urethritis caused by sexually transmitted pathogens)
- Aminoglycosides
The degree of potential toxicity always depends on the developmental stage of the fetus.
More than 40% of pregnancies are unplanned
Considering that over 40% of pregnancies are unplanned, women of childbearing age (20% of the German population) should be regarded as a target group for patients requiring pregnancy-compatible medication.
This is particularly important during early pregnancy (embryonic phase: weeks 3 to 8, when internal and external organs are formed), as the risk of congenital severe malformations and permanent organ damage is highest.
Tip: embryotox.de
The Berlin Charité provides embryotox, an internet portal offering independent information on the safety of medications during pregnancy and breastfeeding. They also offer free, individual consultations.
Most medications are present in breast milk. How much reaches the infant’s system depends on several factors (active ingredient, amount of breast milk, etc.). Some medications, even in minute quantities, can harm the baby.
Young infants under two months (especially preterm infants) are more sensitive to the mother’s (long-term) medication than older infants.
A threshold of 10% of the therapeutic dose has been arbitrarily chosen as a limit for low and clinically insignificant exposure. The exposure index is calculated as the daily dose of the drug consumed by the child (the product of the time-averaged drug concentration in breast milk and the daily breast milk intake – approximately 150 ml/kg body weight) relative to the therapeutic dose.
With many antibiotics, the infant receives less than 1% of the body-weight-adjusted therapeutic dose – these levels are not considered clinically relevant.
Most breastfed infants show no symptoms. In isolated cases, “drug-laden” breast milk may cause looser stools, rarely diarrhoea.
Mothers should generally prefer medications that only need to be taken once a day. These should be taken before the infant’s longest sleep period or immediately after breastfeeding.
Similar to during pregnancy, Pivmecillinam, Penicillins, Cephalosporins, and Macrolides are preferred.
Furthermore, the following antibiotics are also possible during breastfeeding:
- Fosfomycin: After a single dose of Fosfomycin, breastfeeding can continue without interruption.
- Amoxicillin and Clavulanic acid: Depending on the pathogen spectrum, the combination of Amoxicillin and Clavulanic acid can be used during breastfeeding.
- Cotrimoxazole: If required by the pathogen spectrum, breastfeeding can also continue with Cotrimoxazole.
- Ciprofloxacin: If required by the pathogen spectrum, breastfeeding can also continue with Ciprofloxacin.
- Nitrofurantoin: If Nitrofurantoin therapy is absolutely necessary, breastfeeding can continue with this medication. Since only a small amount of Nitrofurantoin passes into breast milk, a bladder infection during breastfeeding should preferably be treated with other substances.
After pregnancy, it's often before pregnancy
Even while breastfeeding, a new pregnancy can occur during the reproductive years. Therefore, when starting a new medication during breastfeeding, pregnancy-compatible drugs should be preferred.
Beware of resistances
Although a wide range of antibiotics is classified as safe during breastfeeding, the discussion about the potential development of resistant pathogens in infants is not yet concluded.
Fact: A small amount of the medication passes into the breast milk and to the baby.
Unclear: To what extent this small amount contributes to the development of resistance.
Tip: embryotox.de
The Charité in Berlin provides embryotox independent information on the safety of medications during pregnancy and breastfeeding on their website. They also offer free individual consultations.
One thing upfront: Before starting antibiotic therapy, a urine culture must always be taken in children to identify the pathogen and determine appropriate antibiotics (=> antibiogram).
If an antibiotic is needed before receiving the antibiogram (=> calculated/empiric therapy), the selection depends on the local resistance situation and the child's age. After receiving the antibiogram (which can take a few days), treatment is tailored according to the age and antibiogram-guided monotherapy.
The dosing is age- and weight-dependent.
Very ill children and newborns receive antibiotics via intramuscular injection or intravenously. Other children take antibiotics orally. The treatment usually lasts 7 to 10 days.
First-line antibiotics according to guidelines:
- Trimethoprim (with or without Sulfamethoxazole) for E. coli resistance rates below 20% (Infectotrimet®, Lidaprim®, Bactrim®, Cotrim®)
- Amoxicillin/Clavulanic acid (e.g. Xiclav®, Amoxiclav®, Clavamox®, Augmentin®)
- Nitrofurantoin (after the 3rd month of life, e.g. Furadantin®, Nifurantin®)
- from 6 years: Pivmecillinam (e.g. Selexid®, X-Systo®)
- from 12 years: Fosfomycin (e.g. Monuril®)
- from 14 years: Nitroxolin
According to guidelines, highly effective reserve antibiotics (e.g. Ciprofloxacin and 2nd or 3rd generation Cephalosporins - Ceftriaxone, Cefotaxime or Ceftazidime) should generally not be used to treat uncomplicated cystitis in children and adolescents. And although Cefaclor seems particularly suitable, it should not be prescribed for uncomplicated cystitis in children and adolescents, if possible.
The reason for this: Resistance development with Cephalosporins. The impact of Cephalosporins on the selection of ESBL (Extended Spectrum Beta-Lactamase) producing bacteria, which are increasingly found in paediatric urinary tract infections according to the guidelines, is particularly problematic. Cephalosporins are highly effective antibiotics whose potency must also be preserved for infections in other organ systems.
Nevertheless, unfortunately, Cephalosporins have now become standard therapeutics when children are infected with the urinary tract and bladder – possibly involving the kidneys. This is particularly true for regions where there is already a high resistance rate against Trimethoprim, the former standard medication for urinary tract infections.
The sad truth in the end: A 2016 study by BKK unfortunately found that antibiotics are prescribed much more frequently to children than to adults. Furthermore, it is rare that microbiological confirmation through antibiogram is conducted.
Therefore, my appeal to you: Please advocate for your child. Encourage the doctor to send a urine sample to determine which uropathogenic germ (or germs) is causing your child’s issue. This will also clarify which antibiotics will be effective, and it won’t be necessary to indiscriminately use broad-spectrum antibiotics.
If the urinary tract infections keep recurring, essentially "chronic", you can try long-term prophylaxis with antibiotics. By long-term prophylaxis, several things can be meant, e.g. regular intake of AB after intercourse or a daily sustained intake of a reduced dose of AB over a period of 3-12 months.
Suitable antibiotics before or after sex:
- Nitrofurantoin (1x50mg or 1x100mg)
- Fosfomycin (1x3000mg)
- Trimethoprim (1x100mg) => unfortunately, high resistance rates are now widespread
Suitable antibiotics for sustained intake (3-12 months long):
- Nitrofurantoin (1x100mg daily)
- Fosfomycin (3x3g weekly)
Once an antibiotic has been found that is tolerated by the body for long-term use, methenamine (Hiprex) is combined with a dose of 2x1g daily.
Links to articles about antibiotics: Antibiotics Natural Antibiotics
Methenamine is an antimicrobial medication for the treatment and prevention of urinary tract infections.
Taken orally (1g = 1 tablet, morning and evening), methenamine reaches the urine. In this slightly acidic environment, formalin (formaldehyde) is released. This has an antiseptic effect that inhibits bacterial growth and can therefore support the treatment of urinary tract infections. As the antibacterial activity of methenamine is greater in acidic urine, additional acidification of the urine may be necessary.
Methenamine is not licensed in Germany due to the potential carcinogenic formaldehyde content, hence it is also unavailable here. However, it can be purchased online, for example, in Denmark (trade name Haiprex) or England (trade name Hiprex).
In the private clinic on Harley Street 10 in London, treatment includes taking Hiprex together with antibiotics.
When talking about a biofilm, it means bacterial colonies that are shielded by an extracellular polymeric matrix (the biofilm) they produce themselves. The biofilm protects the bacteria from attacks of the immune system and the effects of antibiotics.
In a biofilm, the bacteria can survive in up to 1,500 times higher antibiotic concentrations, as it is difficult for the antibiotic to reach the bacteria. By taking antibiotics, the opposite effect may even occur: The biofilm formation is promoted because many antibiotics harm the protective microbiome (urobiome).
The English website Live UTI Free deals intensively with recurring urinary tract infections and describes the different stages of the life cycle of biofilms, Chronic Urinary Tract Infection vs. Recurrent UTI. It becomes clear and understandable why urinary tract infections recur.
Antibiotic in the form of long-term antibiotic therapy is still a means of choice for recurring HWI. The goal: When the biofilm breaks up in its life cycle and bacteria again enter the bladder, the antibiotic has a chance to fight the bacteria. The renewal of the entire bladder mucosa is a longer process (the lifespan of an urothelial cell can be up to 500 days), therefore the antibiotic must be taken for a longer period (at least 3 months, but usually longer).
More on biofilm inhibitors under Why does the antibiotic not work in acute urinary tract infections?
Nitrofurantoin is a chemotherapeutic agent from the antibiotic group of Nitrofurans and is used in the treatment of uncomplicated(!) urinary tract infections in adults.
- Sensitive against 86% of all pathogens causing uncomplicated cystitis.
- Only for uncomplicated cystitis (works only in the bladder, not in the tissue).
- Better effectiveness with acidic pH of urine.
- Longer antibiotic treatment (5 – 7 days) leads to better results.
- Not recommended for pregnant women in the third trimester (6th – 9th month).
- Not for kidney insufficiency.
- Pulmonary side effects (chronic pulmonary fibrosis, pulmonary edema, acute interstitial pneumonia) especially in older women after more than 12 months of long-term antibiotic treatment.
- => For long-term treatment, monitoring is necessary (lungs, liver, kidneys, nerves, blood).
Nitrofurantoin is a so-called prodrug. Prodrugs are substances that are administered to the patient in an inactive form and only later converted into an active substance in the human body. Nitrofurantoin is activated enzymatically in the bacteria themselves and then damages the bacterial DNA, proteins, and enzymes.
Nitrofurantoin is effective against most gram-positive and gram-negative bacteria that cause urinary tract infections (E. coli, Klebsiella, Enterococcus, Enterobacter, and Staphylococcus). According to resistance studies, Nitrofurantoin is sensitive to 86% of all pathogens causing uncomplicated cystitis. The risk of resistance formation is considered relatively low because the targets of the drug are so diverse.
However, there are two exceptions: Nitrofurans are naturally resistant to Pseudomonas aeruginosa and Proteus mirabilis (and related Providencia).
Nitro works only in the bladder
Antibacterial effective concentrations are only reached in the urine, and the active substance does not penetrate kidney tissue. Therefore, Nitrofurantoin (like Fosfomycin-Trometamol and Pivmecillinam) is only recommended for the treatment of uncomplicated cystitis and for prophylaxis in recurrent urinary tract infections. Nitrofurantoin is not suitable for pyelonephritis (UTI with fever, flank pain may indicate this).
Nitro likes it acidic
Nitrofurantoin works optimally when the pH of the urine is in the acidic range, which is why urine acidifying substances (e.g. ascorbic acid, methionine, methenamine/Hiprex®) are sometimes recommended. Alkalizing medications (or foods), such as Acetazolamide, Thiazides, may reduce the effectiveness of Nitrofurantoin.
Alternatives to Nitro
If Nitrofurantoin cannot be taken, the following alternatives are suitable as first-choice antibiotics for an acute uncomplicated urinary tract infection:
- Nitroxolin (Nitroxolin forte, Nilox® midi)
- Pivmecillinam (Selexid®, X-Systo®)
- Fosfomycin-Trometamol (Monuril®)
- Trimethoprim, only when local resistance rates are less than 20% (Selexid®, X-Systo®)
My Conclusion
Unfortunately, general practitioners still prescribe Nitrofurantoin somewhat hesitantly, even though it is a really effective and generally well-tolerated "antibiotic".
The classic side effects of broad-spectrum antibiotics (gastrointestinal issues => damaged microbiome) do not occur, as its effect is limited to the bladder.
Nitro covers almost all pathogens and is also suitable for long-term use in retarded form (macrocrystalline form) as a prophylactic treatment for recurrent bladder infections.
However, you really need to be careful about: The lung function should be monitored closely with prolonged use => I know several people who had to stop taking Nitro due to lung issues.
No, although Nitrofurantoin is effective against most gram-positive and gram-negative bacteria (in 86% of cases, such as E. coli, Klebsiella, Enterococcus, Enterobacter, and Staphylococcus).
Nitrofurans are naturally resistant to Pseudomonas aeruginosa and Proteus mirabilis (and the related Providencia).
Not effective against kidney involvement: Nitrofurantoin is very effective in the bladder, but it does not penetrate into the renal tissue (achieves no effective concentration). Therefore, if you have a urinary tract infection with fever and/or flank pain, Nitrofurantoin is not indicated.
No, Nitrofurantoin is prescription-only.
However, you don't necessarily need to visit a doctor's surgery to get a prescription. Since 2019, it has been permitted across the EU to obtain a prescription through online consultations.
In addition to Nitrofurantoin, there is another nitrofuran derivative called Furazidin, which is available without a prescription in Poland.
More information can be found under What antibiotics are available without a prescription for cystitis?
The antibacterial Furazidin, a Nitrofuran derivative, is similar to the better-known Nitrofurantoin and is available over-the-counter in Poland. The bacteriostatic mechanism of action (similar to Nitrofurantoin) works against both gram-positive (Staphylococcus epidermidis, Staphylococcus aureus, Staphylococcus faecalis) and gram-negative microorganisms (Enterobacteriaceae – Salmonella, Shygella, Proteus, Klebsiella, Escherichia, Enterobacter etc.) and is used to treat urinary tract, skin and soft tissue infections.
According to study, Nitrofurantoin superior
A 2018 study compared the effectiveness of Nitro and Furazidin against classical uropathogenic pathogens and multi-resistant strains of E. coli and Staphylococcus aureus. In vitro, Furazidin showed a better efficacy (Minimum inhibitory concentration) for the following pathogens:
- Proteus mirabilis
- Klebsiella pneumoniae
- MDR (= multi drug resistant) Staphylococcus aureus
- Escherichia coli
How to get it in the UK?
A successful order of UROFURAGINUM MAX 100 MG X 30 TABL could be placed on Apteka-Zielona.pl. It is a Polish online pharmacy registered in the national register, offering competitive prices compared to other online sellers.
Nitroxolin, like Nitrofurantoin, is used to treat acute and chronic urinary tract infections. It is listed in the S3 guideline as a first-choice antibiotic.
Nitroxolin has a broad spectrum of activity that covers numerous gram-negative and gram-positive bacterial species, including Mycoplasma hominis, Ureaplasma urealyticum (sexually transmitted organisms) and Candida spp. (fungi).
Resistance to the drug is rare, similar to Nitrofurantoin.
Like Nitrofurantoin, Nitroxolin requires an acidic environment for optimal efficacy (best at pH 5.5).
The key differences between Nitroxolin and Nitrofurantoin
- Different mode of action (inhibition of RNA polymerase in Nitroxolin, formation of DNA strand breaks in Nitrofurantoin)
- Nitroxolin is up to 64 times more active than Nitrofurantoin.
My Conclusion
If my infection was caused by Proteus mirabilis, Klebsiella pneumoniae or a multiresistant E. coli, I would definitely prefer Nitroxolin (unless contraindicated).
Fosfomycin (e.g. Monuril) is a true star among antibiotics. So far, very few bacteria are known to be resistant to Fosfomycin.
Fosfomycin inhibits an enzyme that the bacteria need for forming their cell wall, and this causes the bacteria to burst.
Since Fosfomycin is required for the treatment of severe, sometimes life-threatening infections, it should remain a last resort for uncomplicated urinary tract infections (the risk of developing resistance increases with frequent prescription).
It should therefore only be used when Nitrofurantoin, Pivmecillinam, or even Trimethoprim have failed to work, as the patient's symptoms suggest.
Therapy update
I frequently read that a single dose of Fosfomycin-Trometamol is not sufficient to cure cystitis. Also, there are cases where Fosfomycin-Trometamol does not seem to work effectively.
The University Clinic Vienna (Department of Infections and Tropics) has issued a therapy update "Acute Cystitis". It states that two doses of Fosfomycin-Trometamol, given 72 hours apart (not just a single shot), may be necessary to effectively treat cystitis.
- Two doses of Fosfomycin-Trometamol, spaced 72 hours apart, may be more effective than a single dose.
- Effectiveness of Fosfomycin-Trometamol in the urinary bladder model is highly variable.
- Development of resistance has been observed even in vivo studies.
- Individual variations in the absorption and distribution of the active substance in the body (pharmacokinetics).
- Need for further studies to determine the optimal dosage.
Fosfomycin is not a fluoroquinolone.
The fluoroquinolones (ciprofloxacin, levofloxacin, moxifloxacin, etc.) are another class of antibiotic, which belong to the broad-spectrum antibiotics and are considered reserve antibiotics, which should be used primarily in cases of complicated urinary tract infections. Not only because of their wide range of action, but also due to some serious side effects, fluoroquinolones should again be treated as reserve antibiotics.
Fosfomycin can either be administered via the bloodstream as an injection or taken orally. For oral administration, the active ingredient is present in powder or granule form as a combination with Trometamol. With the aid of Trometamol, the active ingredient Fosfomycin can be better absorbed in the gastrointestinal tract.
Fosfomycin-Trometamol is used to treat uncomplicated urinary tract infections, also preventively before surgical interventions on the urinary tract, or for long-term prophylaxis (every 10 days a single dose).
As the active ingredient continuously passes into the bladder through the bloodstream, Toilet visits should not be avoided even shortly after taking Fosfomycin, but are actually beneficial for recovery.
Contraindications/Interactions related to the digestive system:
- Diarrhoea, Vomiting: If you have severe diarrhoea or frequent vomiting, the active ingredient may not reach sufficient levels in the bloodstream.
- Gastric motility: Substances that promote rapid movement of stomach and intestinal contents (e.g. for preventing nausea and vomiting) can affect the absorption of Fosfomycin into the body (e.g. Metoclopramide, Domperidone)
Five days of Nitrofurantoin is superior to a single dose of Fosfomycin, according to the study.
Both Nitrofurantoin and the once-daily Fosfomycin are frequently prescribed for uncomplicated cystitis.
In a multinational study with 513 women (from Switzerland, Poland, and Israel), the two antibiotics were compared: Three times daily 100mg Nitrofurantoin for five days versus a single dose of 3000mg Fosfomycin.
The result: Twenty-eight days after completing treatment, 70% of the Nitrofurantoin group were symptom-free, whereas in the Fosfomycin group, only 58% were symptom-free. Furthermore, in the urine culture, the causative germ was not detectable in 74% of the Nitrofurantoin group, compared to 63% of the Fosfomycin group.
It is suspected that Fosfomycin may be less effective than Nitrofurantoin because widespread use has led to the development of resistance among pathogens.
Fosfomycin single dose may not be sufficient: New studies on the efficacy of a single dose of 3000mg Fosfomycin suggest that this is an insufficient dose, and might even promote resistance. Fosfomycin is a reserve antibiotic: Its broad-spectrum effect is urgently needed for use against multiresistant pathogens, which requires a more cautious approach.
A possible treatment approach: For example, administering 3000mg Fosfomycin every three days for three, six, or even nine days.
As a general rule: The sensitivity of pathogens decreases as antibiotic use increases.
The Problem of Multiresistance
Antibiotics inhibit the growth of bacteria through a variety of different mechanisms (bacteriostatic) or kill them (bactericidal).
BUT: The more frequently bacteria are exposed to a particular antibiotic, the higher the likelihood that they will become resistant to it, rendering the medication ineffective. The problem becomes more serious when a bacterium develops resistance to multiple antibiotics - this is referred to as multidrug-resistant pathogens (e.g. MRSA - methicillin-resistant Staphylococcus aureus), which are difficult to treat.
Once bacteria have developed resistance mechanisms, they can transfer them to another bacterial species (via mobile genetic elements called plasmids). This results in entire bacterial strains becoming resistant to antibiotics and potentially spreading (especially feared in hospitals => "hospital-acquired pathogens").
Why do Antibiotic Resistances Develop?
Antibiotic resistances primarily arise because antibiotics are not used correctly:
- too frequently
- at too low a dose
- for too long (yes, exactly, too long is the problem, because bacteria have more time to develop resistance)
- unnecessarily (e.g. for viral infections)
- careless use in intensive animal farming
As short as possible, as long as necessary
Depending on the severity of the disease, antibiotics should only be used for as short a time as possible (but as long as necessary), as the risk of developing resistance increases with the duration of use.
What can you contribute?
Antibiotic-resistant bacteria pose a danger to us all, as they cause infections that are difficult to treat. If we repeatedly take antibiotics unnecessarily or incorrectly, we contribute to the rise of antibiotic-resistant bacteria, one of the world's greatest health problems.
Do your part by
- questioning every antibiotic use => many uncomplicated UTIs heal without antibiotics
- insisting on a urine culture with antibiotic susceptibility testing => this is the only way to choose the best antibiotic
- not taking reserve antibiotics unnecessarily (e.g. fluoroquinolones)
- strictly following the prescription and taking the antibiotics exactly as directed
- only taking antibiotics prescribed by a doctor => self-medication with antibiotics is not responsible!
Post-antibiotic era 2030
The WHO (World Health Organization) warns that we are heading for an era where antibiotics may only be partially effective or not work at all against bacteria. To counter this, more effort is needed in antibiotic research, and at the same time, the use of antibiotic therapy must become more careful.
For Antibiotic Stewardship (rational and responsible use of antibiotics) to prevail, further education for medical professionals is obviously necessary. According to Statista, the knowledge of European medical professionals regarding antibiotic resistance is quite concerning.
Resistance Mechanisms
First of all, it is important to know that there are two types of resistance mechanisms: natural or acquired resistance.
Natural resistance means that an antibiotic simply cannot work against a germ because, for example, the target site is absent. An example: Mycoplasmas (sexually transmitted) do not have a cell wall => therefore, antibiotics that inhibit cell wall synthesis (e.g. penicillins, fosfomycin) are ineffective. There are other reasons for natural resistance: the antibiotic may either not penetrate the lipid membrane of Gram-negative bacteria or it is immediately pumped out by the bacterium.
Specific examples of natural/intrinsic resistance:
- Proteus mirabilis and Pseudomonas aeruginosa are naturally resistant to nitrofurans.
- Penicillin resistance in Gram-negative bacteria (e.g. E. coli).
- Staphylococcus saprophyticus is intrinsically resistant to Mecillinam (Selexid®, Pivmelam®, X-Systo®).
Acquired resistance means that a bacterium has developed a mechanism that makes one or more antibiotics ineffective.
This phenomenon can also arise naturally => genes can mutate randomly during reproduction, and this may give a bacterium "accidental" resistance.
A much more common cause of acquired resistance is the transfer of genetic material: Bacteria exchange parts of their genetic material (=genes) via so-called resistance plasmids. In this way, a bacterium with resistant properties can pass on its "tool" to another, making the bacteria insensitive to an antibiotic.
Less frequently, genetic material is transferred via viruses (phages) (e.g. penicillin resistance in Staphylococcus aureus through phage transduction).
Irresponsible Use of Antibiotics = Selection Pressure = Resistance
Resistance is an inevitable evolutionary process through mutation and selection. Antibiotics create the selection pressure that promotes the growth of resistant germs.
What is meant by selection pressure? Selection pressure is actually a normal event in nature. It ensures that the "strong" survive and the "weak" perish.
When antibiotics are used, resistant bacteria have an advantage over non-resistant bacteria. While the "harmless" ones are killed or inhibited, the "tough" ones (resistant bacteria) can survive the antibiotic treatment and continue to multiply and spread.
=> The higher the selection pressure (usually antibiotics), the more resistance mechanisms a germ acquires.
If you want to delve further into the topic of antibiotics and resistance, I can recommend the materials from a Swiss symposium on the topic of Infectiology and Hygiene in the Perioperative Setting.
Multidrug-Resistant Pathogens
Multidrug resistance is present when only one or no antibiotic group is still sensitive.
In most cases, this involves an ESBL-producing pathogen. ESBL bacteria ("Extended Beta-Lactamase" or "Beta-lactamase with extended spectrum") can split the beta-lactamase rings of significant antibiotic classes with an enzyme, rendering them ineffective (penicillins, cephalosporins of all generations, and monobactams). These enzymes are most commonly found in typical UTI pathogens such as Escherichia coli and Klebsiella.
ESBL-producing bacteria colonise the intestines. For healthy individuals, the colonisation is usually symptom-free and harmless. However, there is a risk that the resistant intestinal bacteria could spread to other parts of the body, such as the urinary tract.
Multidrug-resistant pathogens (MDR) are especially prevalent in countries with very high antibiotic consumption (e.g. in the Middle East). The high transmission rate of multidrug-resistant pathogens is particularly problematic. Some studies show that, for example, one third of Germans who have travelled to countries with high resistance rates return with an MDR. Among returnees from India, this figure rises to up to 70 percent.
MRSA, EBL & Co
The most important antibiotic-resistant pathogens:
- MRSA (Methicillin-resistant Staphylococcus aureus) => Staphylococcus aureus
- ESBL (Extended-Spectrum Beta-Lactamases) => Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis
- MRGN (multidrug-resistant gram-negative pathogens) => Escherichia coli and Klebsiella pneumoniae, Pseudomonas aeruginosa
- VRE (Vancomycin-resistant Enterococci) => Enterococcus faecium and Enterococcus faecalis
Behind these abbreviations are dangerous pathogens, against which hardly any antibiotics are effective anymore. A growing problem are ESBL-producing bacteria. They deactivate almost all beta-lactams and are not inhibited by Tazobactam or Clavulanic acid.
Avoiding Resistances
If microbes are exposed to suboptimal antibiotic concentrations for an extended period of time, they develop resistance. For this reason, bacteria should be targeted with a high antibiotic dose over the shortest possible time. This contradicts the treatment option of long-term antibiotic therapy for recurrent urinary tract infections, but it is often the last resort for those affected. Regarding the dosage of long-term antibiotics, recommendations differ within Europe: While in Germany, for example, delayed-release Nitrofurantoin is administered at a low dose, in England, it is also used at a normal to high dose over a longer period.
There are a number of measures to avoid resistance: In Switzerland, the project "StAR" (Strategy Antibiotic Resistance) aims to counteract the looming multiresistance crisis. The goal is to ensure the long-term effectiveness of antibiotics for both humans and animals . This not only focuses on the rational use of antibiotics in humans but also addresses the use of antibiotics in agriculture and the spread of excreted antibiotics/MRE in the environment (e.g. in wastewater). Another key area of action: Research & Development => How can proven antibiotics be improved regarding resistance? How can we find new active substances that crack the protective shell (= outer membrane) of bacteria? For information for both healthcare professionals and patients, another website has been created: https://www.antibiotika-richtig-einsetzen.ch/ . It is definitely worth checking out.
Risk of Infection in Hospitals: Every urethra is colonized by all kinds of pathogens, and when a catheter is inserted into the urethra, they can travel up to the bladder or even the kidneys, causing infections.
For more on the topic of resistance avoidance, see What happens when you take unnecessary antibiotics?
Recognising and Treating Resistant Pathogens
Depending on how resistant the pathogens are to antibiotics, treating the infection can become difficult to impossible.
Uncomplicated cystitis with ESBL-producing bacteria can be treated with Nitrofurantoin or Cotrimoxazole.
MRSA: Fosfomycin is used in combination with Vancomycin to treat infections caused by MRSA.
Ideally, along with the diagnosis of "ESBL-producing pathogen" or MRSA, an antibiogram is also available, which should always serve as the basis for targeted antibiotic therapy.
Resistance Situation
- Trimethoprim 22.0%
- Trimethoprim + Sulfamethoxazole 21.4%
- Pivmecillinam 3.0%
- Fosfomycin-Trometamol 0.8%
- Nitrofurantoin 0.4%
The resistance rate against Nitrofurantoin remains consistently below 4.5% in countries where it is frequently used to treat urinary tract infections. No correlation between the use of Nitrofurantoin and increased occurrences of ESBL, MRSA, or VRE has been reported.
Ciprofloxacin therapy increases the risk of colonisation with a CIP-resistant strain after 28 days => with effects on household members.
For a detailed graphical representation of the resistance situation by country, pathogens, and antibiotics on a timeline, I recommend the Resistance Map.
For a detailed report on the resistance situation in Europe 2022, I recommend the document Antimicrobial resistance surveillance in Europe 2022.
Antibiotic resistance is increasing at an alarming rate worldwide. Multiresistant bacteria continue to cause major problems in hospitals.
Alternative treatment options are urgently needed.
Mustard oils for problematic pathogens
Mustard oils (e.g. Angocin®) are recommended as a treatment option when resistant pathogens are detected.
According to various in vitro studies, mustard oils show a broad antibacterial spectrum (both in gram-positive and gram-negative ranges), even against resistant forms of E. coli and problem pathogens such as MRSA. You can find more information in my article Natural Antibiotic .
Bacteriophages - the "good" viruses
Phages are viruses that rely on bacteria as host organisms for reproduction. When a phage finds a suitable host (bacterium), it attaches to it and forces the host to replicate the phage's genetic material inside. New phages are produced and, after the bursting of the bacterium, released. The bacterium is destroyed, and many new phages seek out bacteria to destroy.
The remarkable thing: Bacteriophages are specialized in specific bacteria, meaning they act very specifically on the bacteria they can kill. In contrast to broad-spectrum antibiotics that kill a variety of bacterial strains.
Another advantage: Bacteriophages multiply at the site of infection, as long as bacteria are present. Once there are no more bacteria, the phages are gone as well.
Advantage = Disadvantage: Bacteriophages must exactly match the bacterial pathogen, otherwise, they will ignore it and the infection will not be treated. Therefore, the exact pathogen causing the infection must first be determined (e.g. via a urine culture). Only then can it be checked which phages are effective.
In Eastern European countries such as Georgia, phage therapy has been used for much longer, and large databases of bacteria and phages already exist there. Currently, there is no approval for phages in this country – the requirements in terms of quality and safety have not yet been sufficiently proven (e.g. through randomized controlled clinical trials).
My conclusion: In the Facebook support group Embedded Bladder Infection Help and Exchange there are some women who have successfully fought their recurring (embedded) bladder infections with bacteriophages after a long suffering journey. The process is not as straightforward as an antibiotic treatment. First, a urine sample must be sent to a clinic in Georgia (e.g. the hospital in Tbilisi). There, the pathogens are isolated, and the right phages are found. The phages, in the form of tablets and vaginal suppositories, are then sent back to you by post. The therapy lasts about 3 months.